Ventilator Settings
Ventilator Settings
David Ray Velez, MD
Table of Contents
Typical Initial Settings
Basic Settings
- Rate: 8-12 Breaths per Minute
- May Start Higher for a Patient Being Intubated with Acidosis and Tachypnea
- Tidal Volume: 8 ml/kg x Ideal Body Weight
- Lung Protective Strategy: 4-6 ml/kg x Ideal Body Weight
- Pressure Support: 5-10 cm H2O
- Generally Avoid Pressures > 20 cm H2O or PIP > 30-35
- PEEP: 5-8 cm H2O
- FiO2: 100% and Titrate Down Off ABG and Pulse Oximetry as Able
Advanced Settings
- Trigger Sensitivity: -2 cm H2O
- I/E Ratio: 1:2 or 1:3
- Inspiratory Flow Rate: 60 L/min
Basic Settings
Rate (f/RR)
- Definition: Number of Breaths Delivered per Minute
- Excessively High Rates are Uncomfortable and Cause Decreased Exhalation Time Which Can Cause Increased Mean Airway Pressure and Air Trapping
- “Over-Breathing the Vent”: Refers to When a Patient is Taking More Spontaneous Patient-Triggered Breaths at a Rate Beyond the Set Rate on the Ventilator
Tidal Volume (Vt)
- Used in Volume Controlled Modes
- Definition: Volume of Air Delivered with Each Breath
- Excessively High Volumes Increase Pressure Which Causes Barotrauma
Pressure Support (PS)
- Also Known as “Inspiratory Pressure (PI)” or “Change in Pressure (∆P)”
- Used in Pressure Controlled Modes
- Definition: Additional Pressure Added to PEEP to Cause Inspiration
- Excessively High Pressure Causes Barotrauma
- *Different Ventilator Manufacturers May Use Peak Inspiratory Pressure (PIP) Instead
- Peek Inspiratory Pressure (PIP): Highest Pressure Seen During Inspiration
- PIP = PI + PEEP
Positive End Expiratory Pressure (PEEP)
- Definition: Positive Pressure Remaining in the Airways at the End of Expiration
- Effects:
- Increased Alveolar Recruitment (Prevents Collapse to Maximize Oxygen Transfer)
- Increased Functional Residual Capacity (FRC)
- Increased Compliance
- Complications:
- Increased Mean Airway Pressure
- Increased Pulmonary Vascular Resistance Causes Increased Right Atrial Pressure
- Increased Right Atrial Pressure Decreases Venous Return (Preload) and Cardiac Output
- Auto/Intrinsic PEEP (Air Trapping)
- Complication of Mechanical Ventilation Seen in Asthma/COPD
- *See Ventilator Complications
Fraction of Inspired Oxygen (FiO2)
- Definition: Percentage of Oxygen in Air Delivered to the Patient
- FiO2 of Room Air: 21% (Regardless of Altitude)
- Oxygen Toxicity:
- High Oxygen Levels Produce Reactive Oxygen Species (ROS)
- Lorraine Smith Effect – Lung Damage Occurs with High FiO2 (> 60%) for a Prolonged Period of Time (> 24 Hours)
- Paul Bert Effect – CNS Toxicity from High FiO2 Over a Short Period of Time When Barometric Pressure is High (1.6-4.0 ATA)
Advanced Settings
Trigger Sensitivity
- Definition: The Negative Pressure Required to Initiate a Patient-Triggered Breath
- Normal Setting: -2 cm H2O
- If Too High: Weak Patients are Unable to Trigger Breaths
- Patients with High Auto-PEEP May Have Difficulty Inhaling Enough to Activate the Trigger
- If Too Low: Machine will Auto-Cycle Causing Overinflation
- Issues May Arise in the Diagnosis of Brain Death if Noting Spontaneous Breaths that are Caused by a Low Trigger Setting and are Not Due to a True Inspiratory Effort
- Causes of Auto-Triggering:
- Coughing
- Hiccups
- Shivering
- Seizures
- Strong Cardiogenic Oscillators
- Condensation in the Ventilator Circuit (“Rain Out”)
Inspiratory/Expiratory (I/E) Ratio
- Definition: Ratio of Inspiratory Time to Expiratory Time
- Normal Settings: 1:2 or 1:3
- Patients with Airflow Limitation (Asthma/COPD Exacerbation) Should Have Ratios ≥ 1:4 to Limit Auto-PEEP (Need Longer Expiration Time)
- Either I/E Ratio or Inspiratory Flow Rate Can be Adjusted – But Not Both
Inspiratory Flow Rate
- Definition: Rate of Air Flow Delivered During Inspiration
- Normal Settings: 60 L/min
- Patients with Airflow Limitation (Asthma/COPD Exacerbation) Can Have the Rate Increased Up to 120 L/min to Limit Auto-PEEP
- Either I/E Ratio or Inspiratory Flow Rate Can be Adjusted – But Not Both (Serve Same Function)
Inspiratory Flow Waveforms
- Definition: Negative Pressure Required to Initiate a Patient-Triggered Breath
- Square/Constant Waveform: Flow Rate Remains Constant During Inspiration
- Lower Mean Airway Pressure
- May Be Preferred in Isolated TBI (Lower Pressure Allows Improved Cerebral Venous Drainage)
- Decelerating Waveform: Flow Rate is Highest at Initiation but Decreases Throughout Inspiration
- Lower Peak Airway Pressure
- Higher Mean Airway Pressure
- Improved Oxygenation
- Can Decrease Venous Return and Cardiac Output
- Longer Inspiratory Time
- Shorter Expiratory Time
- Higher Risk for CO2 Retention and Air Trapping (Especially in COPD)
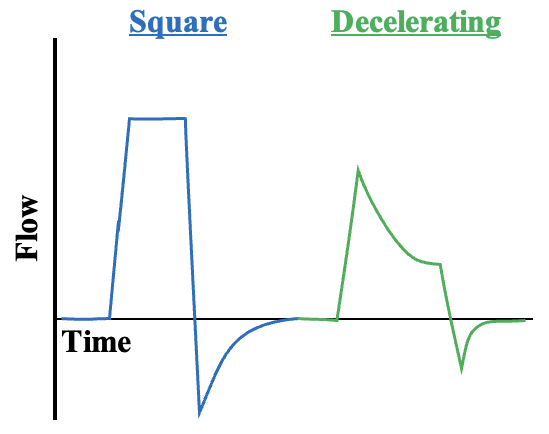
Inspiratory Flow Waveform
