Ureter Trauma
Ureter Trauma
David Ray Velez, MD
Table of Contents
Background
Ureter Injuries in Trauma are Rare
Most Common (95%) After Penetrating Abdominal Trauma
Ureter Trauma is One of the Most Common Sites of Missed Injury at Laparotomy (Rate: 11%)
Missed Injury is Associated with Significant Morbidity (Renal Failure and Sepsis) and Mortality
AAST Ureter Injury Scale
- *See AAST
- Injury Scale is Under Copyright
Diagnosis
Presentation
- Hematuria – An Important Sign but Unreliable (Absent in 67% of Blunt Abdominal Trauma and 45% of Penetrating Abdominal Trauma)
- Flank Pain
- Delayed Signs:
- Persistent Pain
- Fever
- Sepsis
- Fistula
- Ileus
Presentation is Often Nonspecific and Diagnosis Requires a High Index of Suspicion
Diagnosis
- May Be Diagnosed Intraoperatively or on Radiographic Imaging
- Radiographic Imaging:
- CT with IV Contrast (Need Delayed Excretory Phase) is Most Common
- May Also Consider an IV Pyelogram (IVP)
- Consider Cystoscopy with Retrograde Pyelography if Needed
- Intraoperative Evaluation:
- Most Often Seen by Direct Visualization
- IV Methylene Blue or Indigo Carmine May Assist
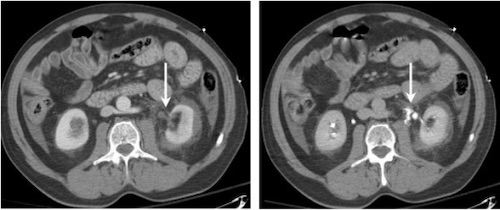
Proximal Ureter Injury with Extravasation (Left); Delayed Imaging (Right) 1
Treatment
The Primary Treatment for Ureter Injury is Surgical Repair
Timing of Repair
- Early Diagnosis (< 3-5 Days): Immediate Repair
- Delayed Diagnosis (> 3-5 Days): Immediate vs Delayed Repair (Controversial)
- Temporize with Endoscopic Stenting vs Percutaneous Nephrostomy Tube if Indicated When Proceeding with Delayed Repair
- Developing Inflammation, Edema, and Friability Increase the Risk of Complications if Attempting Immediate Repair After a Delayed Diagnosis
Definitive Repair
- Upper 2/3 (Over Pelvic Brim): Ureteroureterostomy (Primary Anastomosis)
- Lower 1/3 (Below Pelvic Brim): Ureteroneocystostomy (Reimplant in Bladder)
- *See Techniques Below
Damage Control Options
- Cutaneous Ureterostomy – Stent Placed Through the Proximal Transected Ureter and Externalized to Control Urinary Output Until Stabilized for Delayed Definitive Repair
- Ligate Ends with a Percutaneous Nephrostomy
Surgical Technique
Always Use Absorbable Sutures – Avoid Stricture/Stones
Avoid Skeletonization When Dissecting – Risk for Devascularization
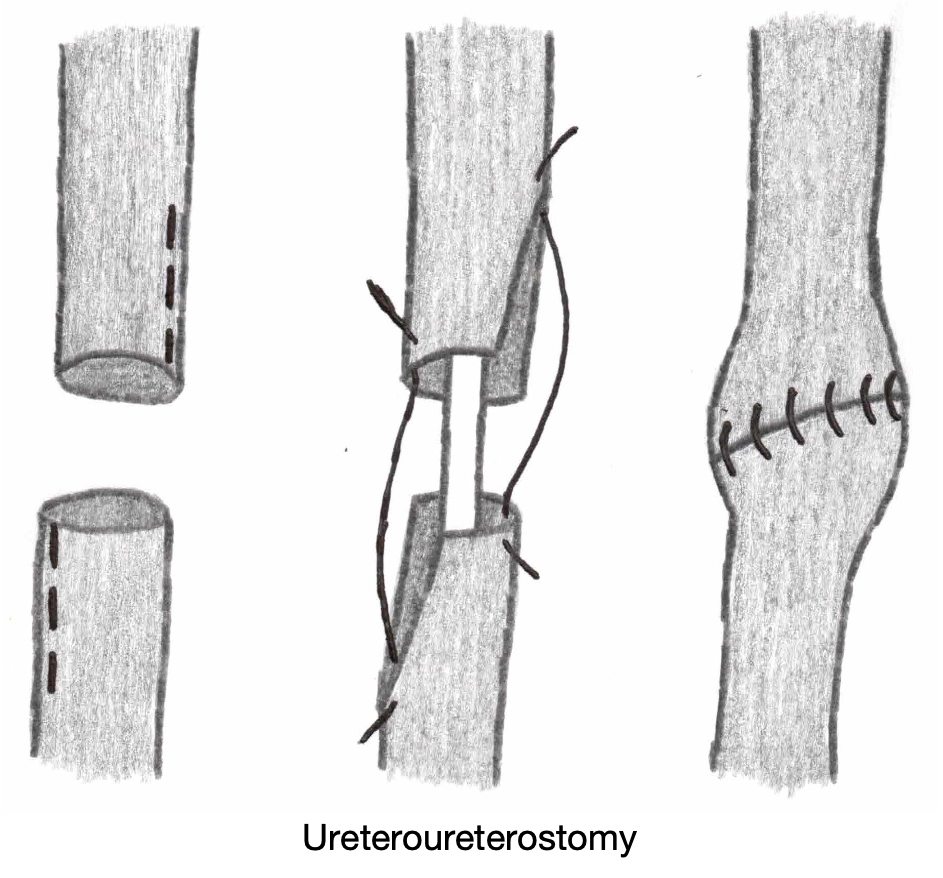
Ureteroureterostomy
- Definition: Ureter-to-Ureter Anastomosis
- Debride Devitalized Tissue
- Spatulate the Proximal and Distal Ends
- Insert a Double-J Ureteral Stent
- Create the Anastomosis Over the Stent
- Use Absorbable Monofilament Sutures (PDS 5-0) to Avoid Stricture/Stones
- *Large Injuries May Require Kidney Mobilization and Nephropexy to Decrease Tension
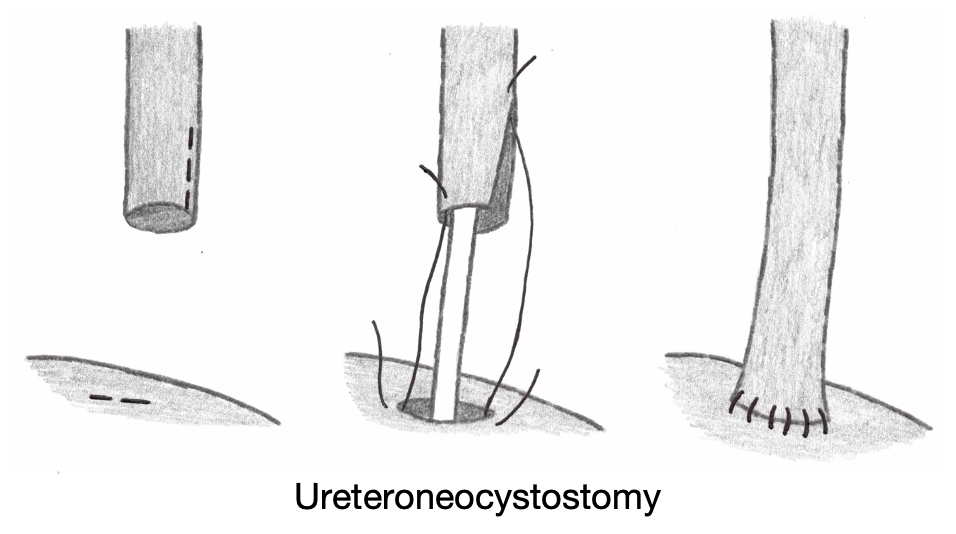
Ureteroneocystostomy
- Definition: Ureter Reimplantation into the Bladder
- Debride Devitalized Tissue
- Spatulate the Proximal End of the Ureter
- Create a Small Cystotomy
- Insert a Double-J Ureteral Stent
- Anastomose the Ureter to the Bladder Cystotomy Over the Stent
- Use Absorbable Monofilament Sutures (PDS 5-0) to Avoid Stricture/Stones
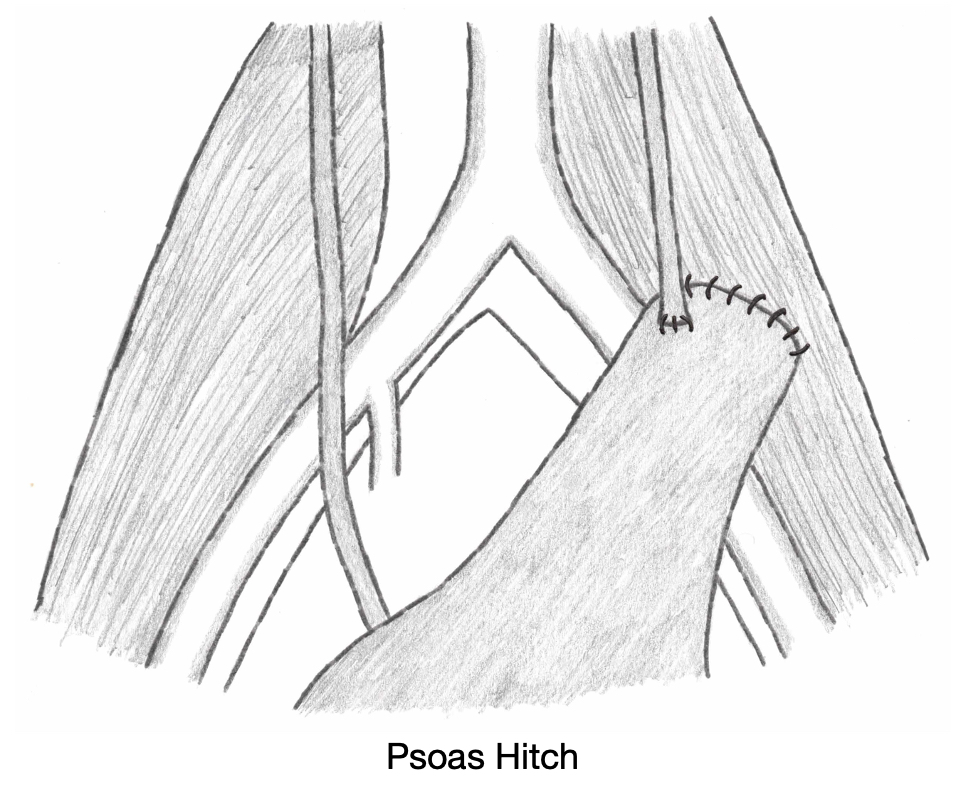
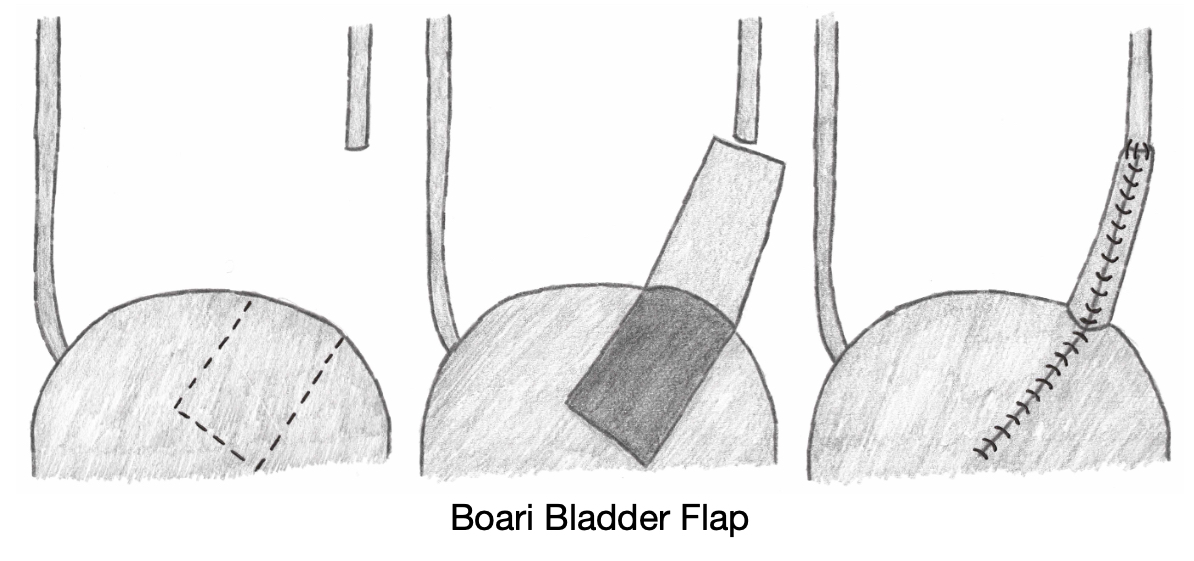
Adjuncts to Decrease Tension for Large Defects
- Psoas Hitch– Mobilize Bladder and Anchor to the Psoas (Generally Preferred)
- Bladder (Boari) Flap – Bladder is Tubularized
- Transureteroureterostomy (TUU) – Implant into the Contralateral Ureter
- Ileal Interposition
- Renal Autotransplantation – Autotransplant of the Ipsilateral Kidney into the Pelvis
References
- Ortega SJ, Netto FS, Hamilton P, Chu P, Tien HC. CT scanning for diagnosing blunt ureteral and ureteropelvic junction injuries. BMC Urol. 2008 Feb 7;8:3. (License: CC BY-2.0)
