Tracheostomy
Tracheostomy
David Ray Velez, MD
Table of Contents
Indications and Timing
Benefits (Compared to Prolonged Endotracheal Intubation)
- More Comfortable and Better Tolerated
- Decreased Work of Breathing
- Decreased Dead Space and Airway Resistance
- Improved Pulmonary Toilet, Oral Care, and Secretion Clearance
- Facilitates Liberation from the Ventilator
- Decreased Ventilatory Dependent Days
- Shorter Hospital Stay
- Shorter ICU Stay
Indications
- Will Require Prolonged Mechanical Ventilation > 7 Days
- Unable to Protect the Airway:
- Unable to Clear Secretions
- Severe TBI
- Severe Maxillofacial Injury
- Severe Neck/Vocal Cord Injury
- Complex Tracheal Repair
- Cervical Spinal Cord Injuries
- Ventilator Dependent Due to Frequent Trips to the OR
Contraindications
- Absolute Contraindications:
- Soft Tissue Infection at the Insertion Site
- Relative Contraindications:
- FiO2 > 60%
- PEEP > 12
- Hemodynamic Instability
- Anatomic or Vascular Abnormalities
- Midline Neck Mass
- Moderate-Severe Coagulopathy
- Morbid Obesity
- Percutaneous Approach is Contraindicated in Infants (Collapsible/Mobile Trachea)
Timing
- Definitions Vary
- Early: Performed within 2-14 Days
- Late: Performed Around 14-21 Days
- Benefits of Early Tracheostomy:
- Higher Likelihood of Ventilator Liberation
- Earlier Return to Walking, Talking, and Eating
- No Change In:
- Ventilator Associated Pneumonia (VAP)
- ICU Length of Stay
- Hospital Length of Stay
- Mortality
- Severe TBI and Cervical Spinal Cord Injuries May Particularly Benefit from Early Tracheostomy
Surgical Approach (Open vs Percutaneous)
- Percutaneous Tracheostomy
- Lower Risk of Surgical Site Infection
- Improved Scar Cosmesis
- Faster Procedure
- Lower Cost
- Similar Bleeding Risk, Decannulation Risk, and Mortality
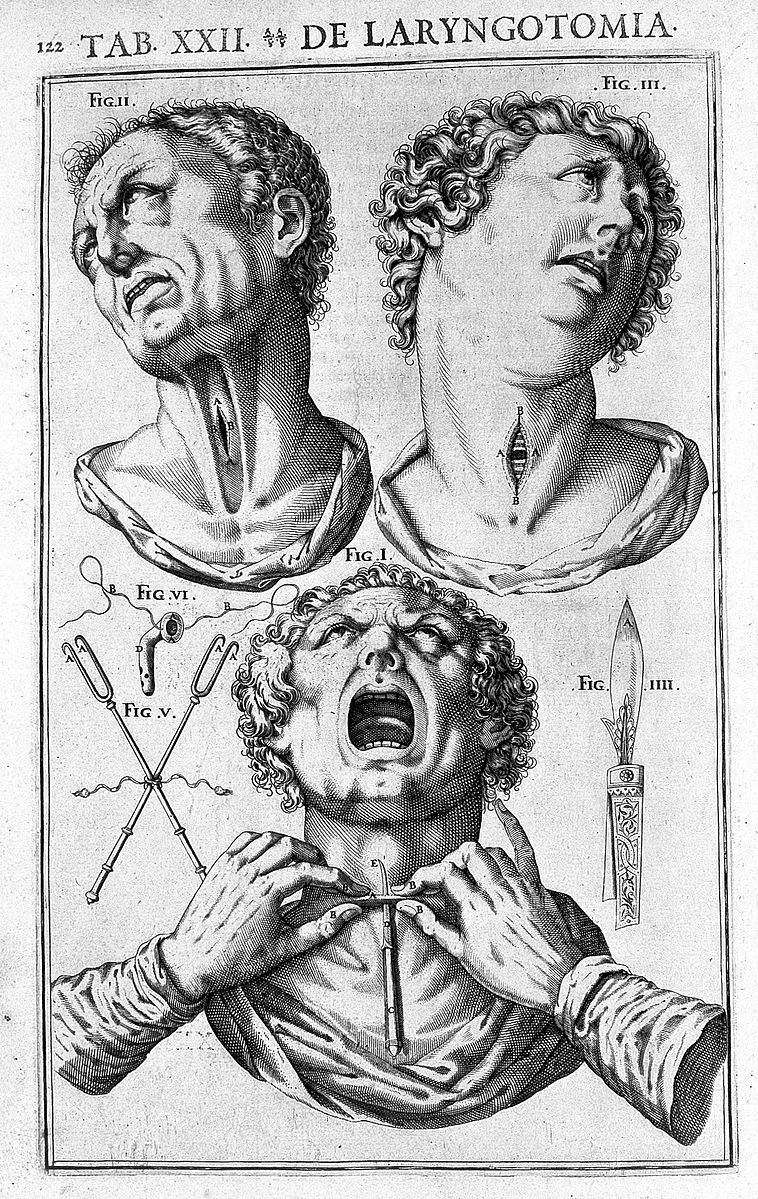
Laryngotomia by Julius Casserius (1552-1616)
Materials and Types
Material
- Shiley (Coviden) – Polyvinyl Chloride (PVC) Plastic
- The Most Commonly Used Material
- Bivona (Portex) – Silicone
- Softer and More Flexible
- Jackson – Metal
- Rarely Used in Modern Practice

Tracheostomy Material: Shiley (Left), Bivona (Middle), Jackson (Right)
Size
- In General, Use the Largest Size Possible for the Initial Placement
- Most Common Sizes:
- Adult Males: 8.0-8.5 mm
- Adult Females: 7.5-8.0 mm
Cuff
- Cuffed: Balloon at the End to Occlude the Surrounding Trachea
- Benefits:
- Allow Secretion Clearance
- Protects from Aspiration
- Allows More Effective PEEP
- Generally Preferred for the Initial Placement
- Cuff Pressure Should Be Maintained at 15-22 mmHg to Avoid Injury (Tracheal Capillary Perfusion Pressure is Normally 25-35 mmHg)
- Benefits:
- Uncuffed: Straight Tip with No Balloon at the End
- Allows Airway Clearance but No Protection from Aspiration
- Used More Commonly in the Long-Term Care and Ventilator Weaning

Tracheostomy Cuff: Cuffed (Left), Uncuffed (Right)
Fenestration
- Has an Additional Opening in the Posterior Tube, Above Any Cuff
- Also Requires a Fenestrated Inner Cannula
- Allows Airflow Past the Tube but Does Not Prevent Aspiration
- Used During the Weaning Process, Generally Not Used for the Initial Placement

Tracheostomy Fenestration: Fenestrated (Left), Non-Fenestrated (Right)
Length
- Standard
- XLT (Extended-Length Tube)
- XLTP – Extra Length Proximally (In-Neck Before the Radial Turn)
- For Swollen/Thick Neck Anatomy
- XLTD – Extra Length Distally (After the Radial Turn into the Trachea)
- For Long Tracheal Anatomy or Tracheal Stenosis
- XLTP – Extra Length Proximally (In-Neck Before the Radial Turn)
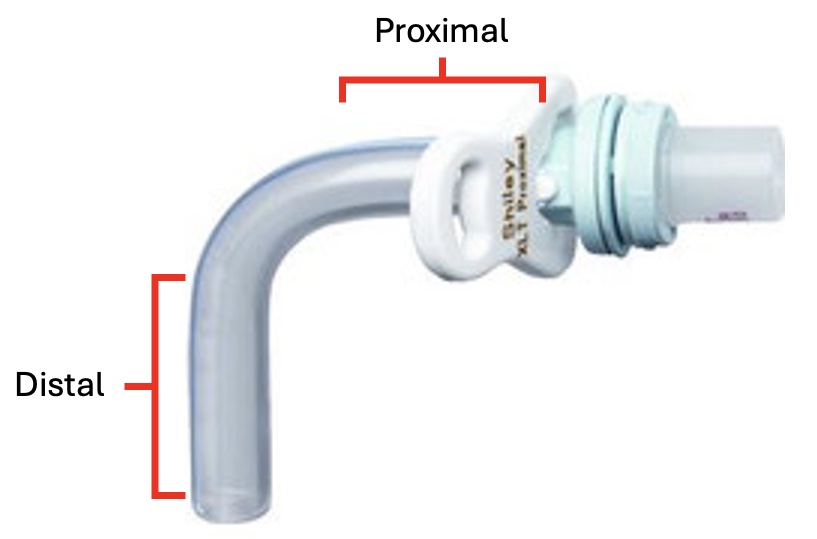
Tracheostomy Length
Complications
Accidental Decannulation/Dislodgement
Bleeding and Tracheoinnominate Fistula (TIF)
Tracheoesophageal Fistula (TEF)
- Risk Factors:
- High Cuff Pressure (#1)
- Concomitant Nasogastric (NG) Tube
- Excessive Motion
- Presentation:
- Ono’s Sign – Uncontrolled Coughing After Swallowing
- Respiratory Distress
- Recurrent Pneumonia
- Initial Management: Large Volume Cuff Endotracheal Tube Below the Fistula to Prevent Aspiration
- Definitive Treatment: Surgical Repair (Primary Repair vs Resection)
- May Consider Combined Tracheal and Esophageal Stenting if Not a Surgical Candidate
- Tracheal Stent Before Esophageal Stent – Esophageal Expansion May Compress the Trachea
- May Consider Combined Tracheal and Esophageal Stenting if Not a Surgical Candidate
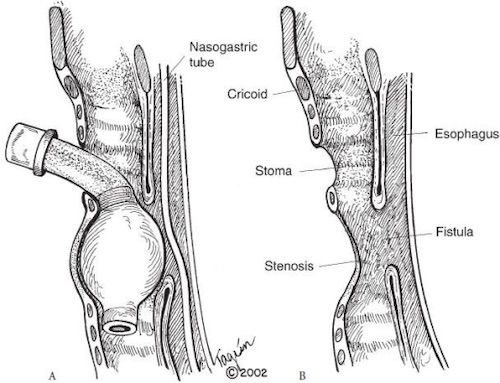
Tracheoesophageal Fistula (TEF) 1
Tracheostomy Obstruction
- Causes:
- Mucous Plugging
- Clotted Blood
- Passage into A False Lumen (Paratracheal Soft Tissue)
- Tube Angulation
- Presentation:
- Acute Respiratory Deterioration
- Elevated Peak Airway Pressures
- Unable to Pass a Suction Catheter Through the Tracheostomy Tube
- Management:
- Can Initially Attempt Suctioning of the Tracheostomy Tube to Clear the Obstruction
- If Suctioning Fails: Exchange the Inner Cannula
- If Exchanging the Inner Cannula Fails or Cannot Be Removed:
- May Attempt Exchanging the Entire Tracheostomy Tube if the Tract is Mature
- Low Threshold to Secure the Airway by Endotracheal Intubation if in Respiratory Distress
Tracheal Stenosis
- The Most Common Late Complication
- Almost All Have Some Degree of Stenosis
- Only 3-12% Have Clinically Significant Stenosis
- Typically Seen at the Level of the Stoma
- Often Asymptomatic Until the Lumen is Reduced to < 5 mm (25-50% of Original Diameter)
- Presentation:
- Elevated Peak Airway Pressures if Infra-Stomal Stenosis
- Dyspnea, Stridor, and Respiratory Failure After Decannulation
- Grading:
- Grade I: ≤ 50%
- Grade II: 51-70%
- Grade III: 71-99%
- Grade IV: 100% (Complete Obstruction)
- Complexity:
- Simple:
- Length < 1 cm
- Only Involves the Mucosa
- Complex:
- Length ≥ 1 cm
- Involves the Cartilage
- Presence of Tracheomalacia
- Simple:
- Diagnosis: Bronchoscopy
- Treatment:
- Simple: Serial Bronchoscopic Dilations
- Possibly Bronchoscopic Resection or Laser Ablation
- Complex: Tracheal Resection (Up to 6 cm) and End-to-End Anastomosis
- Simple: Serial Bronchoscopic Dilations
References
- Paraschiv M. Tracheoesophageal fistula–a complication of prolonged tracheal intubation. J Med Life. 2014 Oct-Dec;7(4):516-21. (License: CC BY-2.0)
