Traumatic Brain Injury (TBI)
Traumatic Brain Injury (TBI)
David Ray Velez, MD
Table of Contents
Types
Epidural Hematoma (EDH)
- Definition: Bleeding Between the Dura Mater and Skull
- Most Common Source: Middle Meningeal Artery
- Often Associated with Temporal Bone Fractures
- CT Appearance:
- Lentiform/Biconvex
- Does Not Cross Midline
- Often Associated with a “Lucid Interval” – A Relatively Normal Period of Time from the Initial Concussion to the Subsequent Coma
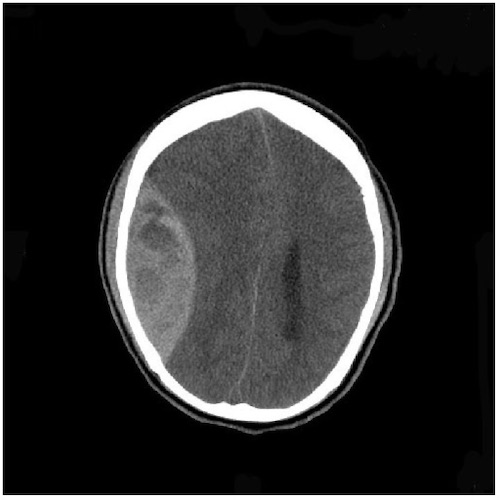
Epidural Hematoma (EDH) 1
Subdural Hematoma (SDH)
- Definition: Bleeding Between the Dura Mater and Arachnoid Mater
- The Most Common Intracranial Hemorrhage
- Source: Venous Plexus/Bridging Veins
- Acceleration/Deceleration Injury
- CT Appearance:
- Crescent-Shaped
- Crosses Midline
- Can Be Chronic in Elderly After Falls
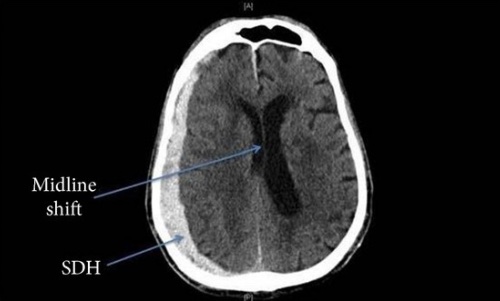
Subdural Hematoma (SDH) 2
Subarachnoid Hemorrhage (SAH)
- Definition: Bleeding Between the Brain and Arachnoid Mater
- Causes:
- Trauma (#1)
- Ruptured Aneurysm (#2)
- Arteriovenous Malformation (AVM)
- Aneurysmal Bleeds are Often Described as a “Thunderclap” Headache that is the “Worst of Life”
- Xanthochromia (Yellow Coloring) of the Cerebrospinal Fluid (CSF) is Pathognomonic
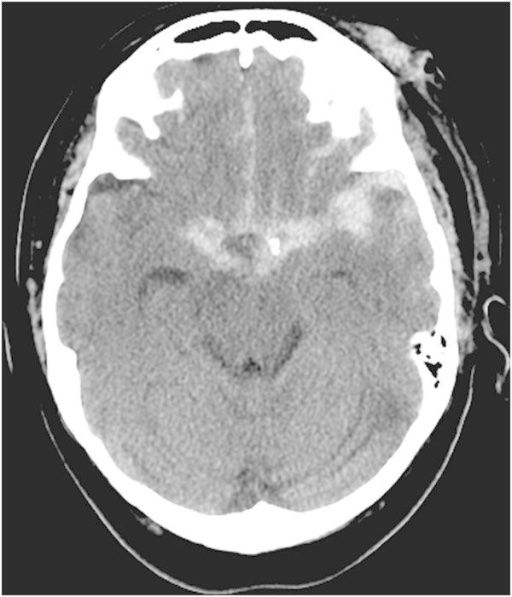
Subarachnoid Hemorrhage (SAH) 3
Diffuse Axonal Injury (DAI)
- Definition: A Diffuse Shearing Injury of the Brain Axons
- Most Common Cause: Rotational Force of Acceleration/Deceleration Impact
- May Not Be Apparent on CT Imaging (Low Diagnostic Yield)
- MRI Appearance:
- Punctate Hemorrhages
- Blurring of Grey-White Interface
- Often Identified Once Patient Has an Original CT Scan on Presentation but Fails to Clinically Improve After 6-24 Hours Prompting an MRI
- Adams Classification:
- Grade 1: Mild DAI with Microscopic White Matter Changes in the Cerebral Cortex, Corpus Callosum, and Brainstem
- Grade 2: Moderate DAI with Gross Focal Lesions in the Corpus Callosum
- Grade 3: Severe DAI with Findings of Grade 2 and Additional Focal Lesions in the Brainstem
- Generally Indicates a Poor Prognosis
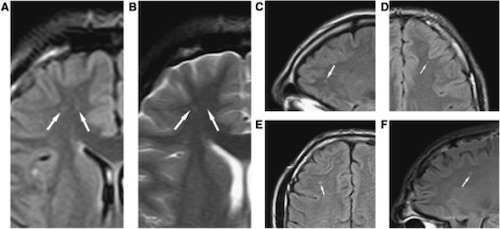
Diffuse Axonal Injury (DAI) on MRI 4
Cerebral Contusion (Parenchymal/Hemorrhagic Contusion)
- Definition: Bruising of the Brain from Multiple Punctate Hemorrhages
- May See Surrounding Edema and Necrosis
- Most Remain Small and Surgically Insignificant
- Often Evolve Over Time and May Worsen or Not Even Be Evident on the Initial CT
- Often See “Coup and Countercoup” Injuries
- “Coup” – Injury at the Site of Head Impact
- “Countercoup” – Injury Remote from the Site of Head Impact (Classically Directly Opposite)
- Most Common Sites: Frontal Base and Anterior Temporal Lobes
Secondary Brain Injury
Definition: Injury That Develops After the Initial/Primary Brain Injury from Metabolic and Physiologic Derangements
Primary Risk Factors
- Hypotension
- Reduced CPP Causes Ischemia
- Autoregulation with Arteriole Vasodilation Causes Increased ICP
- A Single Episode of Hypotension Doubles the Associated Mortality
- Hypoxia
Classification
TBI Classification
- Mild: GCS 13-15
- Moderate: GCS 9-12
- Severe: GCS ≤ 8
Glasgow Coma Scale (GCS)
| # | Motor (6) | Verbal (5) | Eyes (4) |
| 1 | None | None (1T: Intubated) | None |
| 2 | Decerebrate | Incomprehensible | Open to Pain |
| 3 | Decorticate | Inappropriate | Open to Speech |
| 4 | Withdraws to Pain | Confused | Spontaneous |
| 5 | Localizes | Oriented | |
| 6 | Obeys Commands |
Brain Injury Guidelines (BIG)
| Variables | BIG 1 | BIG 2 | BIG 3 |
| LOC | Yes/No | Yes/No | Yes/No |
| Neuro Exam | Normal | Normal | Abnormal |
| Intoxication | No | No/Yes | No/Yes |
| CAP (Coumadin, Aspirin, Plavix) | No | No | Yes |
| Skull Fracture | No | Non-displaced | Displaced |
| SDH | < 4 mm | 5-7 mm | > 8 mm |
| EDH | < 4 mm | 5-7 mm | > 8 mm |
| IPH (Locations) | < 4 mm (x1) | 5-7 mm (x2) | > 8 mm (Multiple) |
| SAH | Trace | Localized | Scattered |
| IVH | No | No | Yes |
Treatment
Basic Management
- Avoid Hypoxia and Hypotension – High Risk for Secondary Brain Injury
- Reverse Any Coagulopathy
- Start Prophylactic Anticoagulation Within 24-48 Hours of a Stable Head CT
- Seizure Prophylaxis: Levetiracetam (Keppra) for 1 Week
- Indicated for Severe TBI (Not Mild-Moderate)
- Reduces Risk of Early Seizures
- No Reduced Risk for Late Seizures or Post-Traumatic Epilepsy
- Fluid Management:
- NS is Generally Preferred Over LR (LR is Relatively Hypotonic and May Worsen Cerebral Edema)
- Avoid Dextrose-Containing Solutions (Worsen Neurologic Injury)
Management Based on BIG Criteria
- BIG 1: Observe for 6 Hours
- BIG 2: Admit and Observe for 24 Hours
- BIG 3: Admit to ICU, Repeat Head CT, and Consult Neurosurgery
Intracranial Pressure (ICP) Monitoring and Management
Surgical Decompression Indications
- Epidural Hematoma (EDH):
- > 30 cc Volume
- GCS ≤ 8 with Pupil Abnormality
- Subdural Hematoma (SDH):
- > 10 mm Thick
- > 5 mm Midline Shift
- GCS ≤ 8 and Decreased by ≥ 2 Since Injury
- GCS ≤ 8 with Pupil Abnormality
- ICP > 20 mmHg
- Subarachnoid Hemorrhage (SAH):
- Posterior Fossa Causing Mass Effects
- > 50 cc Volume
- > 20 cc Volume, > 5 mm Midline Shift, and GCS ≤ 8
Evolving Therapies
- Beta-Blockers (Propranolol)
- Goal: Reduce Blood Pressure and Inhibit Catecholamine Surge-Mediated Inflammation in the Brain
- Exact Role is Still Evolving
- Amantadine (NMDA Antagonist)
- May Improve Cognitive Function After Severe TBI – Clinical Effect Debated
- May Accelerate the Pace of Functional Recovery without Significant Change in the Ultimate Level of Improvement
Two Factors are 100% Specific for Poor Outcome in the Absence of Cofounding Factors:
- Absent or Extensor Motor Response on Day #3
- Absent Pupillary or Corneal Reflexes on Day #3
References
- Yogarajah M, Agu CC, Sivasambu B, Mittler MA. HbSC Disease and Spontaneous Epidural Hematoma with Kernohan’s Notch Phenomena. Case Rep Hematol. 2015;2015:470873. (License: CC BY-3.0)
- Krishnamoorthy V, Sharma D, Prathep S, Vavilala MS. Myocardial dysfunction in acute traumatic brain injury relieved by surgical decompression. Case Rep Anesthesiol. 2013;2013:482596. (License: CC BY-3.0)
- Lasry O, Marcoux J. The use of intravenous Milrinone to treat cerebral vasospasm following traumatic subarachnoid hemorrhage. Springerplus. 2014 Oct 27;3:633. (License: CC BY-4.0)
- Gandy S, Ikonomovic MD, Mitsis E, Elder G, Ahlers ST, Barth J, Stone JR, DeKosky ST. Chronic traumatic encephalopathy: clinical-biomarker correlations and current concepts in pathogenesis. Mol Neurodegener. 2014 Sep 17;9:37. (License: CC BY-2.0)
