Spinal Cord Injury (SCI)
Spinal Cord Injury (SCI)
David Ray Velez, MD
Table of Contents
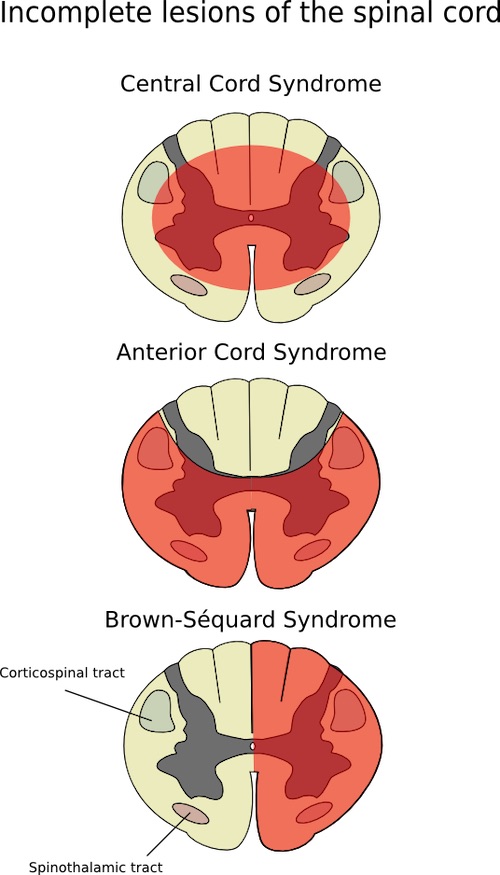
Injury Patterns
Anterior Cord Syndrome
- Injury: Anterior 2/3 of the Spinal Cord
- From Anterior Spinal Artery Injury
- Presentation:
- Bilateral Motor and Pain/Temperature Loss
- Spares Sensation
Brown-Sequard Syndrome
- Injury: Cord Hemisection
- Presentation:
- Ipsilateral Motor and Sensation Loss
- Contralateral Pain/Temperature Loss
Central Cord Syndrome
- Injury: Swelling of the Central Spinal Cord
- From Hyperflexion of C-Spine
- Presentation:
- Bilateral Motor and Pain/Temperature Loss
- “Cape-Like” Distribution Affecting Arms More Than Legs
Cauda Equina Syndrome
- Injury: Compression of the Cauda Equina
- Presentation:
- Saddle Anesthesia
- Bowel/Bladder Dysfunction
- Bilateral Lower Extremity Weakness
Spinal Cord Injury Without Radiographic Abnormality (SCIWORA)
- Newer Term: Spinal Cord Injury Without CT Evidence of Trauma (SCIWOCTET)
- Definition: Clinical Findings of Spinal Cord Injury but Negative XR/CT
- 2/3 Will Have Evidence of Injury by MRI
- Most Common in the Cervical Spine
- Less in the Thoracic Spine Due to Rib Cage Splinting Protection
- Primarily Occurs in Children Due to Increased Elasticity and Proportionally Larger Heads with Weaker Cervical Musculature
- Evaluate with MRI and Manage by Cervical Collar
Spinal Cord Lesions 1
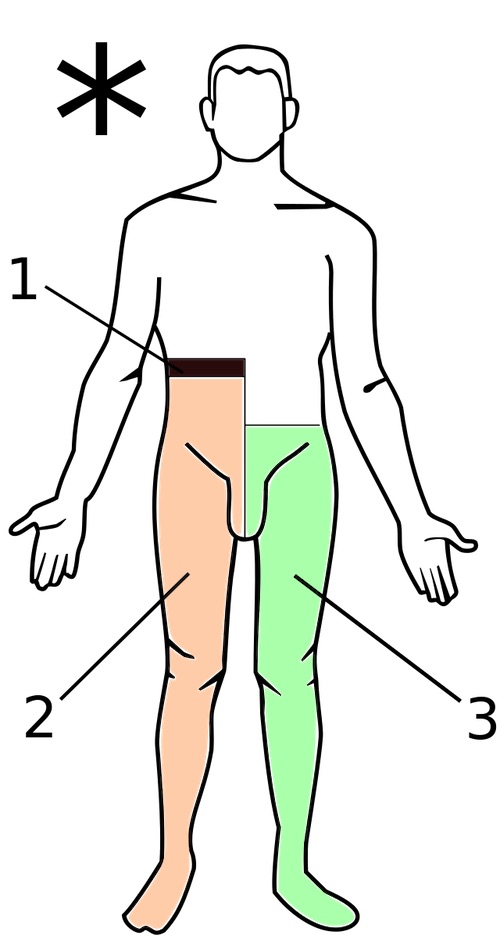
Brown-Sequard: (1) Level of Lesion, (2) Motor/Sensation Loss, (3) Pain/Temperature Loss 2
ASIA Impairment Scale
Grade A Injury
- Complete Injury
- No Sensation or Motor Function in Sacral Segments S4-S5
Grade B Injury
- Sensory Incomplete Injury
- Distal Sensation is Preserved Below the Neurologic Level of Injury and Includes Sacral Segments S4-S5
- No Motor Function ≥ 3 levels Below the Neurologic Level of Injury on Either Side
Grade C Injury
- Motor Incomplete Injury
- Distal Sensation is Preserved Below the Neurologic Level of Injury and Includes Sacral Segments S4-S5
- Distal Motor Function is Preserved Below the Neurologic Level of Injury (> Half of the Key Muscle Functions Have a Muscle Grade < 3)
Grade D Injury
- Motor Incomplete Injury
- Distal Sensation is Preserved Below the Neurologic Level of Injury and Includes Sacral Segments S4-S5
- Distal Motor Function is Preserved Below the Neurologic Level of Injury (≥ Half of the Key Muscle Functions Have a Muscle Grade ≥ 3)
Grade E Injury
- Normal
- Normal Sensation and Motor Function
Spinal Shock
Definition: A Sudden, Temporary Loss of Spinal Cord Function Below the Level of an Injury
- A Sequela of Severe Spinal Cord Injury
Presentation
- Temporary Paralysis, Areflexia, and Loss of Sensation Below the Level of Injury
- Usually Resolves Within 48 Hours but May Last Weeks-to-Months
- No Circulatory Compromise (Compared to Neurogenic Shock)
- Injuries Above T6 May Result in Neurogenic Shock
Pathophysiology
- A Two-Stage Process
- Primary Injury: From the Initial Impact and Continued Cord Compression from Fracture, Ligamentous Injury, and Disc Rupture
- Secondary Injury: Further Injury from Inflammation, Ischemia, Calcium-Mediated Mechanisms, Free Radicals, and Cell Death
Bulbocavernosus Reflex (BCR)
- Also Known As:
- Bulbospongiosus Reflex
- Osinski Reflex
- A Spinal Cord Reflex Involving S1-S3
- Reflex: Anal Sphincter Contraction in Response to Squeezing of the Glans of the Penis, Clitoris, or Tugging on the Foley Catheter
- Carries Prognostic Value:
- Absence of Reflex Demonstrates Continued Spinal Shock – May See More Functional Improvement Once Spinal Shock Resolves
- Presence of Reflex Demonstrates Resolution of Spinal Shock
Neurogenic Shock
Definition: Hemodynamic Shock Caused by a Loss of Sympathetic Tone from Severe Traumatic Brain Injury (TBI) or Spinal Cord Injury
- Seen in Spinal Injuries Above the T6 Level
Incidence
- Cervical Spine Injury: 19.3%
- Thoracic Spine Injury: 7%
Presentation
- Hypotension
- Bradycardia and Bradycardic Arrest
- Bradycardia Can Be Exacerbated by Gastric, Urinary, or Rectal Distention
- Extremities Remain Warm from Vasodilation
- Flushed Skin
- May See Priapism from Vasodilation
General Management
General Management
- Management is Mostly Supportive Outside of Possible Surgery for Spinal Fractures
- Monitor for Cardiovascular and Respiratory Complications in High Spinal Injuries
- Monitor Vital Capacity – Decreases May Indicate Respiratory Failure and Need for Intubation
- High Risk for VTE – May Consider Long-Term Anticoagulation for 2-3 Months
- High Risk for Pressure Sores
Controversial Therapies
- Goal MAP > 85-90 mmHg for 7 Days to Improve Spinal Cord Perfusion Pressure – Poor Quality Evidence to Support
- Systemic Steroids – Primarily Given if Symptoms are Worsening to Decrease Swelling
Treatment of Neurogenic Shock
- Hemodynamic Shock: IV Fluids and Vasopressors
- Vasopressor Choice:
- Norepinephrine – Generally Preferred
- Phenylephrine – May Cause Reflex Bradycardia
- Consider Midodrine for Prolonged Support
- Vasopressor Choice:
- Acute Bradycardia: Atropine, Dopamine, Epinephrine, or External Pacing
- Persistent Bradycardia May Require Permanent Pacemaker Placement
- Additional Supportive Measures to Consider:
- NG Tube Decompression – Gastric Distention Can Exacerbate
- Foley Catheter – Urinary Distention Can Exacerbate
- Bowel Regimen/Rectal Tube – Rectal Distention Can Exacerbate
- Theophylline – Antagonize Endogenous Adenosine at the SA and AV Nodes
- Can Be Used Long-Term and May Be Able to Prevent Pacemaker Placement for Persistent Bradycardia
References
- Olson N. Wikimedia Commons. (License: CC BY-SA-3.0)
- Rhcastilhos, PbBR8498. Wikimedia Commons. (License: CC BY-SA-3.0)
