Rapid Sequence Intubation (RSI)
Rapid Sequence Intubation (RSI)
David Ray Velez, MD
Table of Contents
General Technique
Rapid Sequence Intubation (RSI): A Technique to Induce Immediate Unresponsiveness and Muscular Relaxation to Facilitate Rapid Endotracheal Intubation
- The Fastest and Most Effective Technique to Gain Control of an Emergency Airway
- Mediation Administration is Rapid and Virtually Simultaneous with No Titration
- The Most Common Approach for Emergency Intubation Outside of the Operating Room
Delayed Sequence Intubation (DSI): A Technique for Preoxygenation Prior to Endotracheal Intubation in Which an Induction Agent is Given to Sedate and Allow at Least 3-5 Minutes of Preoxygenation Prior to Paralysis and Intubation
- Used for Patients that are Agitated or Otherwise Intolerant of Preoxygenation
- Ketamine is the Most Commonly Described Induction Agent Given for Sedation (1 mg/kg)
- Requires Extremely Careful Monitoring of Respiratory Status
Apneic Oxygenation: Provide Additional Oxygenation via Nasal Cannula and/or Face Mask After Induction Until Intubation is Achieved
- Increases Minimum Oxygen Saturation but No Change in Risk of Severe Hypoxia, Shock, or Arrest
The “9 P’s” Process for RSI
- Plan
- Prepare – Equipment, Medications, etc.
- Protect the Cervical Spine
- Preoxygenation (Before Drug Administration)
- Pretreatment – Used to Prevent Complications of Airway Manipulation
- Optional for Select Patients
- Paralysis and Induction
- Induction Given BEFORE Paralysis
- Position and Cricoid Pressure
- Placement and Proof
- Postintubation Management
Endotracheal Tube (ETT) Size
- Average Adult Sizing:
- Males: 8.0-8.5 mm
- Females: 7.0-7.5 mm
- Multiple Formulas Exist for Calculating Size Based on Body Height in Adults
- Pediatrics: (Age in Years / 4) + 4
- Can Use the Patient’s Pinky to Estimate Tube Diameter
- *Short Trachea Makes it Easier to Mainstem
Endotracheal Tube (ETT) Cuff
- The Cuff is an Inflatable Balloon at the Distal End of the Endotracheal Tube Used to Prevent Aspiration and Prevent Air Leakage, Facilitating Positive Pressure Ventilation
- The Majority of Endotracheal Tubes are Cuffed
- Use Uncuffed Tubes in Neonates < 1 Year Old
- OK to Use Cuffed Tubes in Older Peds
- *Old Dogma to Not to Use Cuffed Tubes in Pediatrics is Now Forgone Given Newer Tubes with Lower Pressure
Confirmation of Endotracheal Tube Placement
- Techniques:
- End Tidal CO2 (ETCO2) – The Gold Standard and Best Determinant
- Direct Visualization
- Chest Xray
- Esophageal Detector Devices
- Transtracheal US – Can Supplement Patients in Cardiopulmonary Arrest Who May Have Decreased Flow and Falsely Low ETCO2
- Goal Distance: Tip 2-3 cm Above Carina
Pretreatment
General Indications for Pretreatment
- High Airway Pressures
- High Intracranial Pressures (ICP)
- Select Cardiovascular Conditions
- *Mnemonic for Indications for Pretreatment in RSI: “ABC”
- A: Asthma
- B: Brain
- C: Cardiovascular
General Approach
- High Airway Pressures: Albuterol or Lidocaine
- High ICP: Fentanyl
- Cardiovascular Conditions:
- Prevent Hypertension (Acute Coronary Syndrome or Aortic Dissection): Fentanyl
- Prevent Hypotension (Shock): Vasopressors
Medications
- Aerosolized Beta-2 Agonist (Albuterol)
- If Presenting with Acute Bronchospasm
- Lidocaine
- Reduce Risk of Bronchospasm if a Beta-2 Agonist is Not Given
- Dose: 1.5 mg/kg IV Given 3 Minutes Before Induction
- *120 mg for an Average 80 kg Male
- Onset of Action: 45-90 Seconds
- Contraindication: High-Grade Heart Block – Can Cause Cardiac Arrest
- Fentanyl
- Reduce Cardiovascular Effects from Acute Sympathetic Stimulation if Rapid Blood Pressure Rise Would Be Dangerous (High ICP or Cardiovascular Disease)
- Dose: 1.5-3 mcg/kg IV Given 3 Minutes Before Induction
- *120-240 mcg for an Average 80 kg Male
- Vasopressors (Alpha-Adrenergic Agents)
- Given to Patients in Shock to Maintain Blood Pressure and Attempt to Mitigate the Possible Hypotension After Induction
- Dose:
- Epinephrine 5-20 mcg
- Phenylephrine 50-200 mcg
- Atropine
- Used to Prevent Vagally-Induced Bradycardia in Infants (< 1 Year Old)
- Dose: 0.02 mg/kg IV (Maximum 1 mg)
- Small (Defasciculating) Dose of Neuromuscular Blocker
- Was Historically Given Prior to the Use of Succinylcholine to Reduce Rise in ICP from Succinylcholine-Induced Fasciculations
- No Longer Recommended – No Evidence to Support
Induction Agents
Etomidate
- GABA Receptor Agonist
- Dose: 0.3-0.4 mg/kg
- *24-32 mg for an Average 80 kg Male
- Advantages: Minimal Cardiovascular Effects
- Disadvantages: Can Cause Adrenocortical Suppression
- Primarily Concerned If Given by Long-Term Continuous Infusion and Less So When Given as a Bolus Dose in RSI
Ketamine
- Noncompetitive NMDA Receptor Antagonist
- Dose: 1-2 mg/kg
- *80-160 mg for an Average 80 kg Male
- Advantages: Stimulates Catecholamine Release, Bronchodilation, and Has No Significant Respiratory Depression
- Disadvantages: Catecholamine Release Can Cause Tachycardia, Hypertension, and Increased Myocardial Oxygen Consumption
- Avoid in Severe Cardiac Decompensation (MI or Unstable Angina)
- Can Also Cause Hallucinations
- *Historically Contraindicated in TBI Due to Increased Cerebral Blood Flow and ICP – Now Disproven
Midazolam
- GABA Receptor Agonist
- Dose: 0.2-0.3 mg/kg – Commonly Underdosed
- *16-24 mg for an Average 80 kg Male
- Advantages: Added Amnesic Effects
- Disadvantages: Respiratory Depression and Hypotension
Propofol
- GABA Receptor Agonist
- Dose: 1.5-3 mg/kg
- *120-240 mg for an Average 80 kg Male
- Advantages: Bronchodilation and Decreased ICP
- Disadvantages: Significant Cardiovascular Effects (Hypotension and Bradycardia)
Paralytic Agents
Rocuronium
- Non-Depolarizing Agent
- Dose: 1.0-1.2 mg/kg IV
- *80-96 mg for an Average 80 kg Male
- Onset of Action: 45-60 Seconds
- Duration of Action: 45 Minutes
- Contraindicated if Needing Rapid Recovery (Neuro Assessment or Elective Procedures)
Succinylcholine
- Depolarizing Agent
- Dose: 1.5 mg/kg IV
- *120 mg for an Average 80 kg Male
- Onset of Action: 45-60 Seconds
- Duration of Action: 10 Minutes
- Many Contraindications:
- Hyperkalemia
- Burns (> 3-5 Days)
- Rhabdomyolysis
- Malignant Hyperthermia
- Neuromuscular Disease
*Most Other Paralytic Drugs Have Too Delayed an Onset of Action for RSI
Laryngoscopy
Direct Laryngoscopy: Use of a Laryngoscope to Directly Visualize the Vocal Cords for Endotracheal Intubation
Indirect Laryngoscopy: Examination of the Larynx without a Direct Ling-of-Sight (Ex: Using Light and Small Tilted Mirrors) – Used for Diagnostics and Not for Endotracheal Intubation
Video Laryngoscopy: Use of Fiberoptic Videoscopic Guidance to Allow Better Visualization of the Vocal Cords for Endotracheal Intubation
Levitan Approach
- Position and Preparation
- Identify the Epiglottis
- Laryngeal Exposure
- Place the Tube
Laryngoscope Blades
- Macintosh (Mac) Blade
- Curved Blade with a 90-Degree Handle
- Tip is Placed in Vallecula (Between the Tongue and Epiglottis)
- Sizes:
- Macintosh 3 – The Standard Original Size
- Macintosh 4 – A Larger Size for Bigger Patients
- Macintosh 1 and 2 – Smaller Sizes for Pediatric Patients
- Mac is the Most Commonly Used Blade
- Miller Blade
- Straight Blade with Curved Tip
- Tip is Placed Under the Epiglottis
- Other Less Commonly Used:
- Kessel – Curved with 110-Degree Handle
- McCoy – Curved with a Flexible Distal Tip
Video Laryngoscopy
- Fiberoptic Videoscopic Guidance Allows Better Visualization
- Some Consider it to be “Standard of Care” – Heatedly Debated
- Examples: GlideScope, Storz C-Mac, etc.
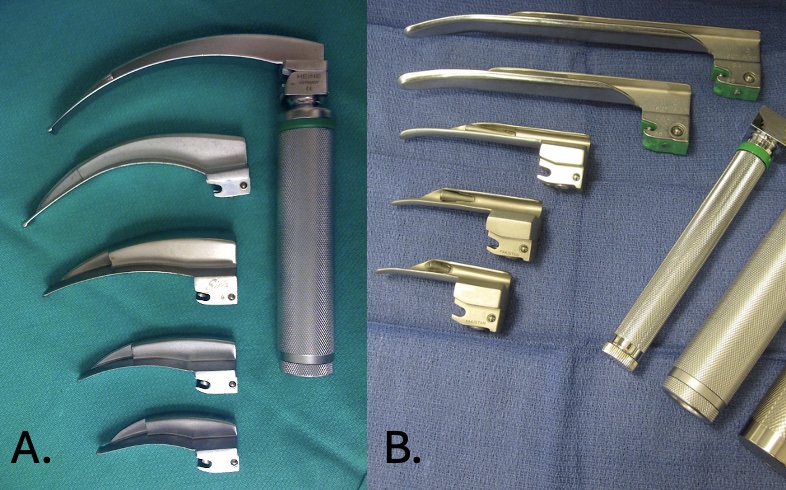
Laryngoscope Blades: (A) Mac 1, (B) Miller 2
Rescue Techniques
Cricoid Pressure (Sellick Maneuver)
- External Digital Pressure Applied to the Cricoid Cartilage
- May Prevent Passive Regurgitation of Gastric Contents (No Real Evidence)
- Generally Does Not Assist is Visualization
- May Actually Inhibit View and Compress the Airway, Blocking Tube Passage
Video Laryngoscopy
- Fiberoptic Videoscopic Guidance to Allow Better Visualization
- Can Be Used as a Rescue Technique if Not Already Using as the Primary Technique for Intubation
Flexible Bougies
- Bent Thin Semi-Rigid Stylette that is Easier to Place Initially than a Larger Endotracheal Tube
- Placement:
- Bougie is First Placed Through the Cords into the Trachea
- Produces “Washboard Effect” as it Rubs Against Tracheal Rings to Confirm Placement
- Endotracheal Tube Then Advanced Over the Bougie into Place
Laryngeal Mask Airway (LMA)
- Elliptical Cuff with Tip Occluding the Esophagus
- Creates Low Pressure Seal Around the Larynx
- Not a Definitive Airway Protection and Does Not Ensure Patency
Combitube
- Dual Lumen Esophagotracheal Tube
- One Tube in Esophagus
- One Tube in Trachea
- May Be Helpful in Select Circumstances
Emergency Cricothyroidotomy
- *See Cricothyroidotomy
- Contraindicated for Pediatrics Under Age 10-12 Years
- *Instead Consider Needle Cricothyroidotomy
References
- Macintosh Blades. Sasata. Wikimedia Commons. (License: CC BY-3.0)
- Miller Blades. DiverDave. Wikimedia Commons. (License: CC BY-3.0)