Resuscitative Thoracotomy
Resuscitative Thoracotomy
David Ray Velez, MD
Table of Contents
Goals and Outcomes
Indications
Procedure/Technique
Additional Measures
Also Known as: “ED Thoracotomy” or “ER Thoracotomy”
Goals and Outcomes
Goals
- Immediately Restore Cardiac Output
- Release Pericardial Tamponade
- Perform Open Cardiac Massage
- Control Major Thoracic Hemorrhage
- Temporarily Occlude the Descending Thoracic Aorta
- Evacuate Massive Air Embolism
Survival/Outcomes
- Overall: 7.4-8.5%
- Penetrating Trauma: 9.0-15.0%
- Isolated Penetrating Cardiac Injury: 17.3-35.0% – Best Outcomes
- Penetrating Abdominal Injury: 4.0-7.0%
- Blunt Trauma: 1.4-2.7%
Indications
General Indications
- Blunt Trauma with Signs of Life After Injury and CPR < 10 Minutes
- Penetrating Torso Trauma with CPR < 15 Minutes
- Penetrating Non-Torso Trauma with CPR < 5 Minutes
Western Trauma Association (WTA) Algorithm (2012)
- CPR with No Signs of Life:
- Penetrating Trauma:
- < 15 Minutes of Prehospital CPR
- < 5 Minutes of Prehospital CPR with Penetrating Trauma to the Neck or Extremity
- Blunt Trauma:
- < 10 Minutes of Prehospital CPR
- Penetrating Trauma:
- Consider for Profound Refractory Shock (CPR with Signs of Life or SBP < 60 mmHg)
EAST Guidelines (2015)
- Penetrating Trauma:
- Thoracic Injury
- Pulseless with Signs of Life After Injury – Strong Recommendation
- Pulseless without Signs of Life After Injury – Conditional Recommendation
- Extra-Thoracic Injury
- Pulseless with Signs of Life After Injury – Conditional Recommendation
- Pulseless without Signs of Life After Injury – Conditional Recommendation
- Thoracic Injury
- Blunt Trauma:
- Pulseless with Signs of Life After Injury – Conditional Recommendation
- Pulseless without Signs of Life After Injury – Recommend Against
Western Trauma Association (WTA) Algorithm (2024 Update)
- Profound Shock (SBP < 60 mmHg) and No Improvement with Initial Measures
- Arrest with Signs of Life (SOL) on Arrival
- *If Cardiac Electrical Activity/PEA is the Only SOL, Only Perform if Tamponade is Present
- *May Still Consider, But Less Well Indicated for Head, Neck, or Extremity Injury
- Arrest with No Signs of Life on Arrival:
- Penetrating Trauma with < 15 Minutes CPR and Tamponade
- Blunt Trauma with < 10 Minutes CPR and Tamponade
- Defined Signs of Life (SOL):
- Pupillary Response
- Spontaneous Ventilation
- Presence of a Pulse or Measurable Blood Pressure
- Extremity Movement
- Electrical Cardiac Activity
- *This is Significantly Simplified and the 2024 Updates are Much More Complex
Procedure/Technique
General Approach
- Incision
- Open Pericardial Sac – Typically the First Step
- ACLS Measures as Indicated
- Cardiac Massage
- Internal Defibrillation
- Intracardiac Epinephrine
- Cross-Clamp Aorta
- Control Any Overt Hemorrhage
- Aspiration if Air Embolism Suspected
- *Order May Vary Depending on Presentation
Incision
- Left Anterolateral Thoracotomy (Some Prefer a “Clamshell” Bilateral Anterolateral Thoracotomy)
- Place Left Arm Above the Head
- Incision at the Left Intercostal Space #4-5
- Just Under the Nipple or Inframammary Fold
- Extend from the Sternum All the Way Down to the Bed Along the Curvature of the Rib
- Enter Along Superior Margin of Lower Rib Using a Curved Mayo Scissors to Cut Through the Intercostals
- Use a Rib Spreader (Finochietto Retractor) to Retract
Pericardiotomy/Open Pericardial Sac
- Open Pericardium Anterior and Parallel to the Phrenic Nerve
- Evacuate Any Pericardial Clot
- Control Any Active Bleeding
- Digital Pressure on Ventricles or Vascular Clamps on Atrium
- Definitive Repair May Be Delayed Until Initial Resuscitation is Complete
- *Always Open – Some Consider it Acceptable to Skip if No Tamponade or There Are Obvious Non-Cardiac Injuries
Cardiac Massage and Internal Defibrillation
- Cardiac Massage
- Induced Cardiac Output:
- External Compressions: 20-25% of Baseline
- Internal Massage: 60-70% of Baseline
- Two-Hand Hinged “Clapping” Technique
- Do Not Use Fingertips or One-Hand with the Thumb Which May Penetrate the Myocardium
- Induced Cardiac Output:
- Internal Defibrillation (If in Ventricular Fibrillation)
- One Paddle on the Anterior Surface and One on the Posterior Surface
- Maximum of 50 J – Do Not Need to “Clear” from Touching the Patient Due to Low Energy
- Also Consider Intracardiac Epinephrine to the Left Ventricle
Cross-Clamp the Aorta
- Indicated if Hypotension (SBP < 70 mmHg) Persists After Pericardiotomy
- Retract the Left Lung Superiorly and Anteriorly
- May Need to Divide the Inferior Pulmonary Ligament (Risks Injury to the Inferior Pulmonary Vein)
- Dissect the Thoracic Aorta
- Incise the Mediastinal Pleura
- Bluntly Separate the Esophagus from the Aorta
- Esophagus Lies Anterior to the Aorta
- Consider Orogastric Tube Placement to Assist in Differentiation
- Take Care to Avoid Cross-Clamping the Esophagus
- Both May Appears Flaccid in Hypotensive Patient Making Identification Difficult
- Bluntly Separate the Aorta from the Posterior Vertebrae
- Clamp the Aorta Just Above the Diaphragm
- Use a Large DeBakey or Satinsky Clamp
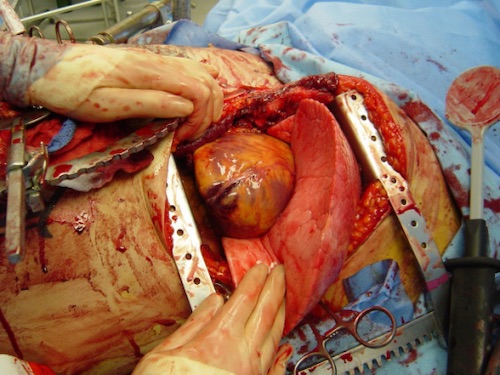
Finochietto Retractor 1
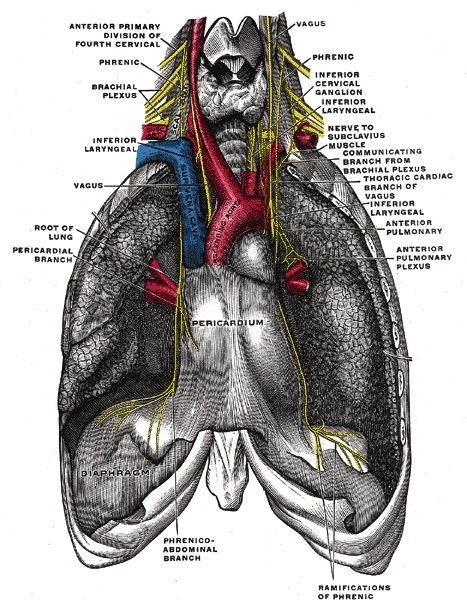
Pericardium and Phrenic Nerve Anatomy 2
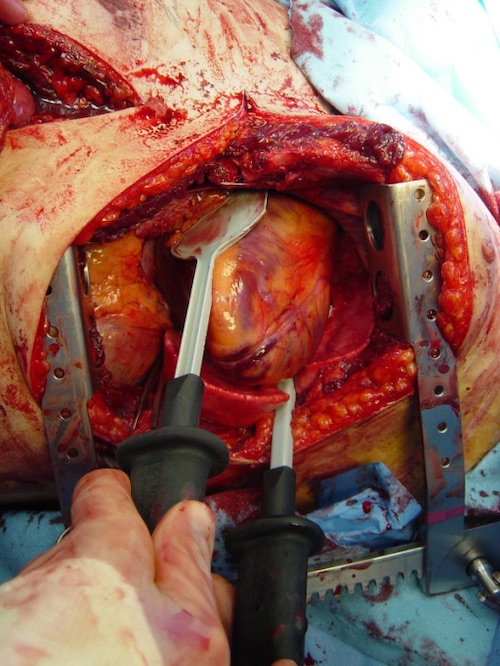
Internal Defibrillation 1
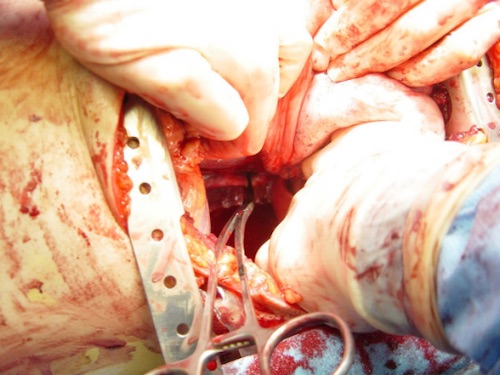
Aorta Cross-Clamp 1
Additional Measures
Anesthesiology Can Right Main-Stem the Endotracheal Tube to Reduce Left Lung Ventilation if Necessary for Visualization and Access
Control Hemorrhage
- Cardiac Injury
- Control Injury to the Heart First
- Often Use 3-0 Prolene (Non-Absorbable)
- Often Perform Simple Running in the Atrium and Vertical Mattress in the Ventricles
- May Require Buttressing with Teflon or Pericardial Pledgets
- Lung Injury
- Can Clamp Parenchyma
- Can Clamp Hilum (From Superior to Inferior – Does Not Require Mobilization)
- “Pulmonary Hilar Twist”
- First Divide the Inferior Pulmonary Ligament
- Rotate the Lower Lobe Anteriorly Over the Upper Lobe
- *Last Choice – High Morbidity and May Require Pneumonectomy if Maintained for Prolonged Periods of Time
- Control Any Other Obvious Sites of Bleeding
Evacuate Air Embolism
- Air Embolism May Occur From Traumatic Bronchovenous Communications
- Due to Relatively High Bronchoalveolar Pressure and Low Pulmonary Venous Pressure
- Often Seen as Acute Decompensation Shortly After Intubation and Positive-Pressure Ventilation
- Cross-Clamp the Hilum of the Suspected Source to Prevent Propagation
- Place in Trendelenburg Position
- Aspirate Air from the Apex of the Left Ventricle and Aortic Root
References
- Cothren CC, Moore EE. Emergency department thoracotomy for the critically injured patient: Objectives, indications, and outcomes. World J Emerg Surg. 2006 Mar 24;1:4. (License: CC BY-2.0)
- Gray H. Anatomy of the Human Body (1918). Public Domain.
