Pneumothorax (PTX)
Pneumothorax (PTX)
David Ray Velez, MD
Table of Contents
Definitions
Pneumothorax (PTX): Gas within the Pleural Space Between the Lungs and Chest Wall
Occult Pneumothorax: A Pneumothorax Seen on CT but Not Visible on Chest X-Ray
Causes
- Traumatic Pneumothorax: Pneumothorax Due to an External Event
- After Penetrating Injury 80% Have Concomitant Hemothorax (Hemopneumothorax)
- Spontaneous Pneumothorax: Pneumothorax without Any External Event
Cardiopulmonary Effect
- Simple Pneumothorax: Pneumothorax Not Causing Compromise of Cardiac or Pulmonary Function
- Tension Pneumothorax: Life-Threatening Pneumothorax Causing Compromise of Cardiac and Pulmonary Function
- Mediastinal Shift Causes Decreased Venous Return and Circulatory Collapse
- Tension Pneumothorax is a Clinical Diagnosis
Chest Wall
- Open Pneumothorax: Trauma Creates a Hole in the Chest Wall, Allowing Air from the Environment to Enter into the Pleural Cavity
- “Sucking Chest Wound”: Refers to a Specific Type of Open Pneumothorax in Which Air is Audibly Sucked into the Pleural Space Through the Chest Wound, Creating a Distinctive “Sucking” Sound
- May Open on Inspiration and Close on Expiration – Increasing the Size without the Opportunity to Expel the Air (High Risk for Tension Pneumothorax)
- Closed Pneumothorax: Pneumothorax without an Open Hole in the Chest Wall and Air Enters from the Lungs
Size
- Small Pneumothorax: ≤ 3 cm at the Apex or ≤ 2 cm at the Hilum
- Large Pneumothorax: > 3 cm at the Apex or > 2 cm at the Hilum
Pneumothorax (PTX)
Spontaneous Pneumothorax
Types
- Primary: No Underlying Clinical Lung Disease
- Secondary: From Underlying Clinical Lung Disease
Secondary Causes
- COPD/Emphysema – Most Common Cause (50-70%)
- Risk Correlates to Severity of Disease
- Interstitial Lung Disease
- Malignancy
- Tuberculosis (TB)
- Sarcoidosis
- Cystic Fibrosis
- Catamenial Pneumothorax
- Pneumothorax Associated with Menstruation
- Due to Thoracic Endometriosis
- Necrotizing Pneumonia
Risk Factors
- Male (3-6x Higher)
- Smoking
- Age:
- Primary – Generally Younger (10-30 Years)
- Secondary – Generally Older (> 55 Years)
- Family History
- Profession (Airline Pilots and Scuba-Divers)
- Marfan Syndrome
- Homocystinuria
- Thoracic Endometriosis
- Malnutrition
- *Classic Patient with Primary Spontaneous Pneumothorax: Healthy, Thin, Tall, Young Male
Association with COVID
- An Uncommon Complication
- Incidence of Cystic Changes in the Lung: 10%
- Incidence of Spontaneous Pneumothorax: 0.66%
- Predominant Risk Factor: Mechanical Ventilation
- Pathophysiology:
- Cytokine Storm – Hyperactive and Dysregulated Immune Response Causes a Hyperinflammatory form of ARDS
- Thrombosis and Microangiopathy
- Pneumatocele May Be Due to Diffuse Alveolar Damage and Necrosis of Airway Walls
Pathophysiology
- Almost All are Due to Rupture of Subpleural Bleb/Bullae
- Cause of Both Primary and Secondary Disease
- Most Common Site: Right Upper Lobe Apex
Diagnosis
Simple Pneumothorax is Most Often Diagnosed on Imaging (CT is the Gold Standard)
Tension Pneumothorax is a Clinical Diagnosis
Physical Exam Findings
- Unequal Breath Sounds (Decreased/Absent on the Affected Side)
- Hyperresonance (Hollow Sound) to Percussion
- Adventitious Lung Sounds (Crackles/Wheezing on the Affected Side)
- Decreased Chest Wall Movement
- Crepitance (Subcutaneous Emphysema)
- Respiratory Distress
- Tachypnea
- Signs of Tension Physiology:
- Jugular Venous Distention (JVD)
- Hypotension
- Tracheal Deviation – Away from the Affected Side
- Hypoxemia
- Cyanosis
Chest X-Ray (CXR) Sensitivity
- Upright: 92%
- Supine: 50%
- *20% of “Occult” Pneumothoraxes in Trauma was Actually “Missed”
General Radiographic Findings:
- Pleural Line Separating Lung from Chest Wall
- Loss of Normal Lung Markings to the Peripheral Chest Wall
Radiographic Signs in a Supine CXR:
- Deep Sulcus Sign: Abnormally Deepened Ipsilateral Costophrenic Angle
- Seen on Supine CXR Because Air Collects Anteriorly/Basally
- The Most Commonly “Missed” Sign
- COPD Can Cause a False Deep Sulcus Sign Due to Hyperinflation
- Relative Lucency of Ipsilateral Hemithorax
- Increased Sharpness of Cardiac Border, Mediastinal Margin or Diaphragm
- Depression of the Ipsilateral Hemidiaphragm
- Double Diaphragm Sign: Visualization of the Anterior Costophrenic Sulcus (Due to Air) and the Diaphragmatic Dome (Due to Lung Border)
- Pericardial Fat Tag Sign: Nodular Contour of the Cardiac Border
- Due to Change in Shape of the Pericardial Fat that is No Longer Compressed by the Lung
Point-of-Care Ultrasound (POCUS)
- eFAST Sensitivity: 92-100%
- Positive eFAST May Still Be Occult and Does Not Definitively Require Chest Tube Placement if Stable and CXR is Negative
- Lung Sliding: Movement of the Two Pleural Layers During Respiration
- Indicates that the Two Layers are in Apposition
- Represents a Normal Finding
- Absent Lung Sliding Can Be Due to Pneumothorax or Pleural Effusion
- Lung Sliding on M-Mode:
- Seashore Sign: Pleura and Chest Wall Appear as Horizontal Lines (Sea) While Lung Parenchyma Appears as Grainy Sand (Shore)
- Indicates Lung Sliding and Represents Normal Parenchyma
- Barcode (Stratosphere) Sign: Entirely Uniform Horizontal Lines (Resembling a Barcode)
- Indicates a Lack of Underlying Lung Sliding Concerning for Pneumothorax
- Lung Point: The Interface Between Normal Lung Tissue (With Lung Sliding) and a Pneumothorax (Absent Sliding)
- Used to Evaluate the Size of a Pneumothorax – More Lateral/Posterior Lung Point Indicates a Larger Size
- Seashore Sign: Pleura and Chest Wall Appear as Horizontal Lines (Sea) While Lung Parenchyma Appears as Grainy Sand (Shore)

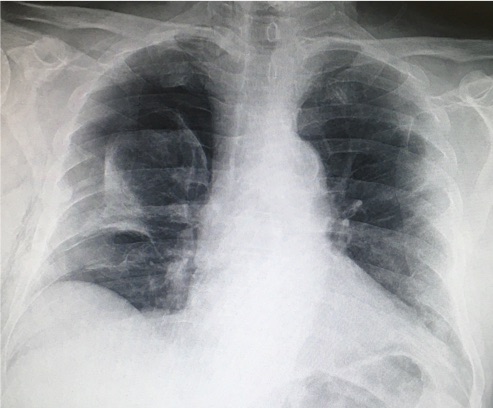
Pneumothorax Causing Mediastinal Shift on CT

Deep Sulcus Sign (Right) on Supine CXR 1
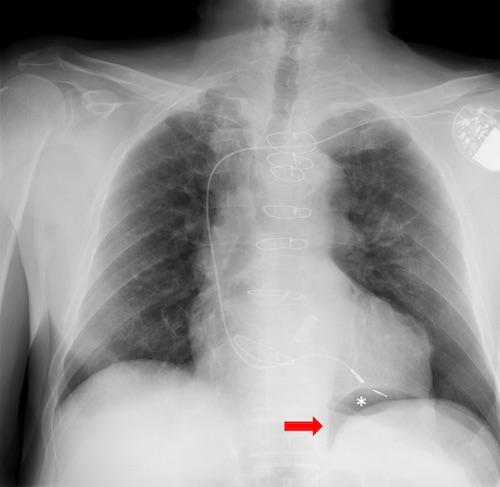
Double Diaphragm Sign (Asterisk) on Supine CXR 2
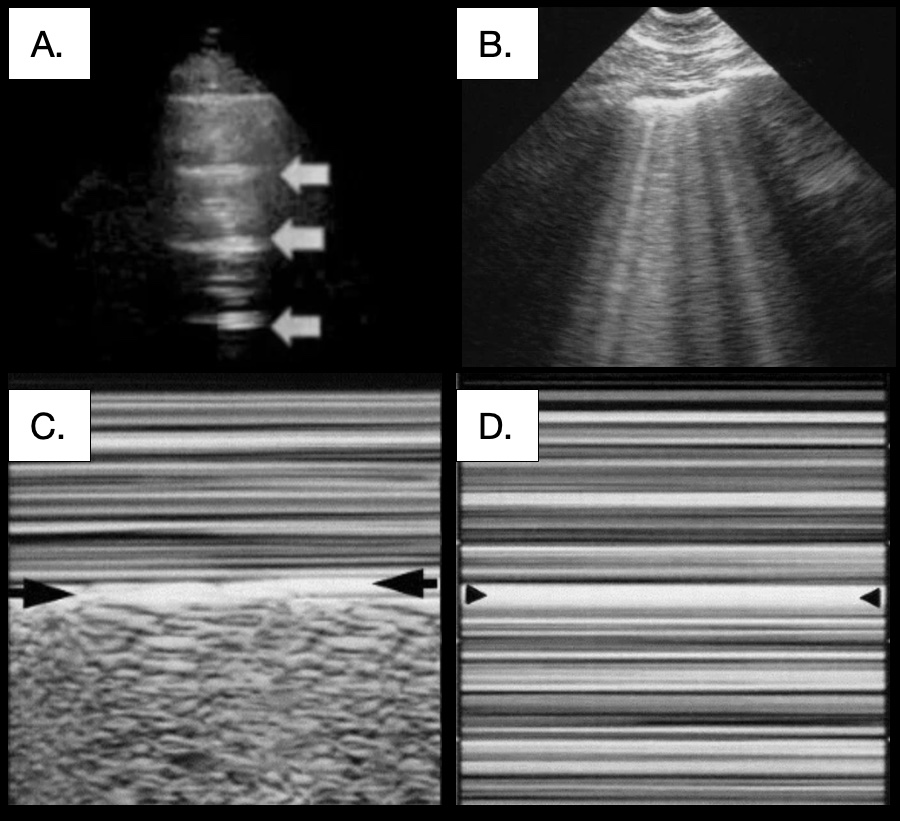
Pulmonary POCUS: (A) A-Lines (Arrows) 3; (B) B-Lines 4; (C) Seashore Sign 4; (D) Barcode Sign 4
Treatment
Simple Pneumothorax
- Asymptomatic and Small (< 3 cm): Observation
- Repeat CXR in 6 Hours to Monitor Progression
- Supplemental Oxygen May Enhance Reabsorption – Reduces Partial Pressure of Nitrogen for a Diffusion Gradient
- Symptomatic or Large (> 3 cm): Chest Tube
- *See Thoracostomy Tube (Chest Tube)
- Smaller Tubes (8-14 Fr) are Generally Preferred for Pneumothoraxes
- *Some Propose Conservative Management Even for Moderate-Large Size Spontaneous Pneumothoraxes if Asymptomatic (Debated)
Tension Pneumothorax
- Requires Emergent Chest Tube Placement
- A Clinical Diagnosis – Do Not Wait for CXR
- Consider Needle Thoracostomy (Needle Decompression) if Chest Tube Placement Will Cause Any Delay
- Should Follow Up Needle Decompression with a Chest Tube Once Able
- Large Bore (14 Gauge) Needle Through the Midaxillary Line at the 4th/5th Intercostal Space
- *Historically Placed at the 2nd/3rd Intercostal Space at the Midclavicular Line – Higher Risk of Failing to Actually Penetrate the Pleural Cavity
Open Pneumothorax (Sucking Chest Wound)
- Place Chest Tube at a Distant Site (Same Site Risks Infection)
- Create an Occlusive Dressing “Taped on 3 Sides”
- Allows Air to Escape on Expiration (Through the Open Side) but Not Enter on Inspiration (Negative Pressure Pulls Dressing in to Occlude the Opening)
Persistent Air Leak (PAL)
Persistent Air Leak (PAL) Definition: Air Leak > 5-7 Days
Indicates an Alveolar-Pleural Fistula or Bronchopleural Fistula (BPF)
Complications
- Poor Lung Expansion
- Ventilation/Perfusion (V:Q) Mismatch
- Direct Extension of Pulmonary Infection into the Pleural Space
- Unable to Maintain Positive End-Expiratory Pressure (PEEP)
- Increased Risk of Pneumonia
- Higher ICU Readmission
- Longer Hospital Length of Stay
Risk Factors
- COPD
- Smoker
- Diabetes
- Female Sex
- Low FEV1
- Steroids
Cerfolio Classification
- Grade 1 (FE): During Forced Expiration Only (Cough)
- Grade 2 (E): Only During Expiration
- Grade 3 (I): Only During Inspiration
- Grade 4 (C): Continuous During Both Inspiration and Expiration
Decrease the Pressure Gradient
- Limit Positive Pressure Ventilation or Extubate if Appropriate
- Chest Tube Water Seal vs Suction is Debated
- Water Seal – Decrease Flow of Air Through the Defect
- Suction – Removes Air from the Pleural Space Faster than the Air Leakage Promoting Pleural Apposition to Promote Healing
Treatment
- Surgery is the Mainstay of Treatment of PAL
- Video-Assisted Thoracoscopic Surgery (VATS) is Generally Preferred Over Open Thoracotomy
- Resect Any Visible Blebs or Bullae and Perform Mechanical Pleurodesis to Achieve Pleural Symphysis
- If No Blebs are Seen – Still Preform an Apical Resection
- Options if Not a Surgical Candidate:
- Chemical Pleurodesis
- Chemical Sclerosants Instilled Through a Chest Tube to Induce an Inflammatory Response to Seal the Pleural Space
- Chemical Options: Talc, Doxycycline, Tetracycline, Bleomycin
- Requires Visceral and Parietal Pleural Apposition (Minimal-to-No Residual Pneumothorax) to Seal – Sclerosis May Prevent Lung Expansion Otherwise
- Complications: Significant Pain, Fever, Lung Injury, and Empyema
- One-Way Flutter Valve (Heimlich Valve)
- Allows Air to Escape but Not Enter
- Can Be Continued in the Outpatient Setting
- Bronchoscopy
- Options: Sealants, Sclerosants, or One-Way Valves (Intrabronchial Valve/IBV)
- Techniques are Evolving
- Chemical Pleurodesis
References
- Kohli MD, Rosenman M. Indiana University.2013. (License: CC BY-NC-ND-4.0)
- Moreno SA, et al. Thoracic Trauma: A Comprehensive Review of Radiological Findings. ECR 2015. Poster C-2031. DOI: 10.1594/ecr2015/C-2031. (License: Open Liscence – Not Specified)
- Gargani L, Volpicelli G. How I do it: lung ultrasound. Cardiovasc Ultrasound. 2014 Jul 4;12:25. (License: CC BY-4.0)
- Lichtenstein DA. Lung ultrasound in the critically ill. Ann Intensive Care. 2014 Jan 9;4(1):1. (License: CC BY-2.0)
