Point-of-Care Ultrasound (POCUS)
Point-of-Care Ultrasound (POCUS)
David Ray Velez, MD
Table of Contents
Point-of-Care Ultrasound (POCUS)
Definition
- Definition: Advanced Diagnostic Ultrasonography Performed and Interpreted by the Physician at Bedside
- More Rapid Use and Results are Optimal in the Critical Care Setting When Formal Diagnostic Imaging May Delay Diagnosis and Treatment
- Highly Operator Dependent
Applications and Assessment
- Cardiac Ultrasound
- Regional Wall Motion Abnormalities or Global Hypokinesis
- Calculate Left Ventricular Ejection Fraction (LVEF)
- Pericardial Fluid
- Right Ventricular Function and Evaluate for Pulmonary Embolism
- Inferior Vena Cava (IVC) Ultrasound
- Fluid Responsiveness
- Pulmonary Ultrasound
- Pleural Effusion
- Pneumothorax (PTX)
- Pulmonary Edema or Pneumonia
- Abdominal Ultrasound
- Cholelithiasis and Cholecystitis
- Appendicitis
- Intussusception
- Hydronephrosis
- Focused Assessment with Sonography for Trauma (FAST)
- *See Focused Assessment with Sonography for Trauma (FAST)
- Gestational Age
- Vascular Ultrasound
- Deep venous Thrombosis (DVT)
- Abdominal Aortic Aneurysm (AAA)
- Ultrasound-Guided Peripheral and Central Venous Catheters
- Skin and Soft Tissue Ultrasound
- Abscess
- Soft Tissue Mass
- Foreign Body
Cardiac Ultrasound
Four Primary Views
- Using a Phased-Array Probe
- Parasternal Long-Axis View (PLAX): Left Sternal Border at the 3rd-4th Intercostal Space, Probe Indicator to the Right Shoulder
- Parasternal Short-Axis View (PSAX): Left Sternal Border at the 3rd-4th Intercostal Space, Probe Indicator to the Left Shoulder
- Apical 4-Chamber View (A4C): Just Inferior to the Left Nipple, Probe Indicator to the Left Flank
- Subcostal View: 2-3 cm Below the Xyphoid
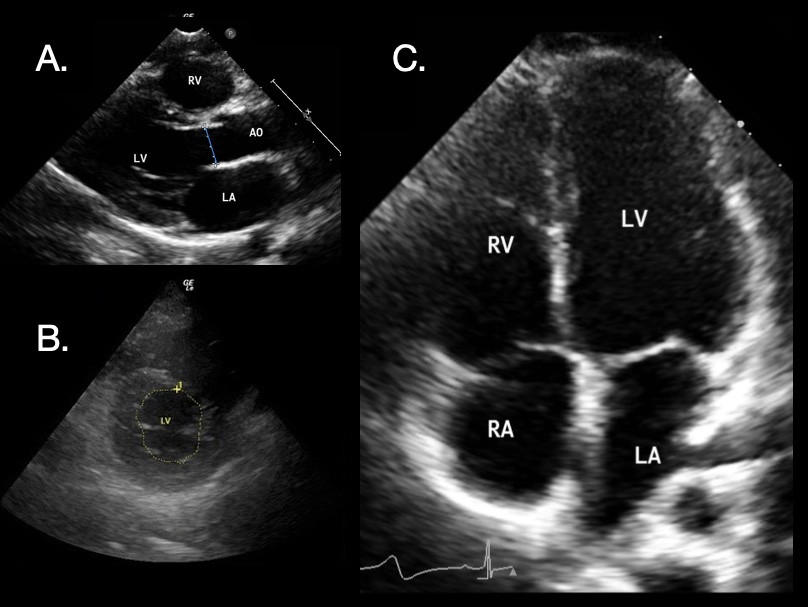
Cardiac POCUS: (A) Parasternal Long-Axis 1; (B) Parasternal Short-Axis 2; (C) Apical 4-Chamber 1 [Right Atrium (RA), Right Ventricle (RV), Left Atrium (LA), Left Ventricle (LV), Aortic Outflow (AO)]
Left Ventricle (LV) Evaluation
- Evaluate for Regional Wall Motion Abnormalities or Global Hypokinesis
- Evaluate Ejection Fraction (Normal 50-70%)
- Qualitative Assessment of EF:
- Left Ventricle Wall Movement
- Anterior Mitral Valve Movement
- Quantitative Assessment of EF:
- E-Point Septal Separation (EPSS): Estimates LVEF By Assessing Mitral Valve Leaflet Movement Toward the Ventricular Septum
- Fractional Shortening: Estimates LVEF By Assessing Change in Diameter of the LV
- Fractional Area Change: Estimates LVEF By Assessing Change in Cross-Sectional Area of the LV
- Simpson (Biplane) Method: Estimates LVEF By Assessing Change in Volume of the LV
- *See POCUS: Left Ventricular Ejection Fraction (LVEF)
Right Ventricle (RV) Evaluation
- Evaluate for Regional Wall Motion Abnormalities or Global Hypokinesis
- D-Sign: LV is “D” Shaped Due to Flattening of the Interventricular Septum from RV Overload
- Normally the LV is Round with RV Wrapped Around it on Parasternal Short-Axis View
- Tricuspid Annular Plane Systolic Excursion (TAPSE): A4C View Using M Mode to Quantify the Tricuspid Annulus Movement Toward the Apex
- TAPSE < 16 mm Indicates Poor RV Function
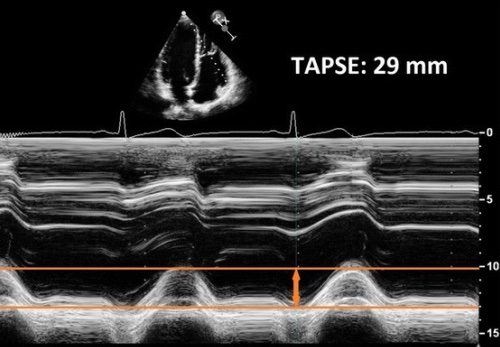
TAPSE on POCUS 3
Pericardial Effusion
- Dark Hypoechoic Fluid Seen Around the Heart
- Best Seen in Parasternal Long-Axis or Subcostal View
- Differentiate from Pathology with a Similar Appearance:
- Pericardial Fat Pad – Usually Located Anteriorly and Will Not Be Completely Anechoic (Pericardial Effusion May Be More Circumferential and More Hypoechoic)
- Pleural Effusion – Will Be Seen Posterior to the Descending Aorta (Pericardial Effusion is Seen Anterior to the Descending Aorta)
- Signs of Cardiac Tamponade:
- Systolic Right Atrial Collapse – First Sign
- Diastolic Right Ventricular Collapse
- Dilated and Noncollapsible IVC
- “Swinging Heart” with Pendular Motion from Circumferential Fluid Accumulation
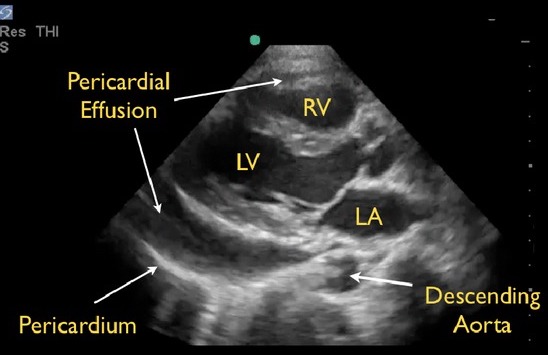
Pericardial Effusion on POCUS: Anterior to the Descending Aorta 4
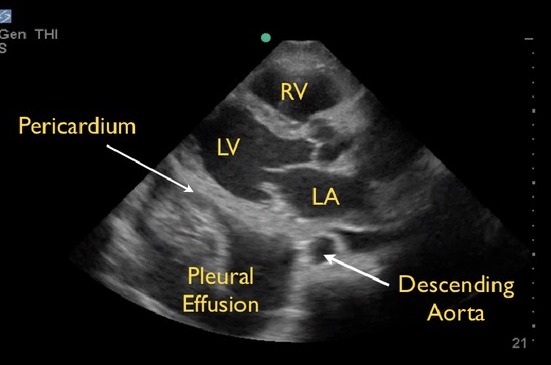
Pleural Effusion on POCUS: Posterior to the Descending Aorta 4
POCUS Evaluation for Pulmonary Embolism (PE)
- Left Ventricle (LV): Normal Function
- Right Ventricle (RV): Severely Dilated with Reduced Systolic Function and Wall Hypokinesis
- Septal Flattening (From RV Pressure Overload)
- Pulmonary Artery Hypertension
- McConnell Sign: RV Dysfunction with Akinesia of the Mid-Free Wall but Normal Motion at the Apex
- Highly Specific for PE
- D-Sign: Left Ventricle is “D” Shaped Due to Flattening of the Interventricular Septum from Right Ventricular Overload
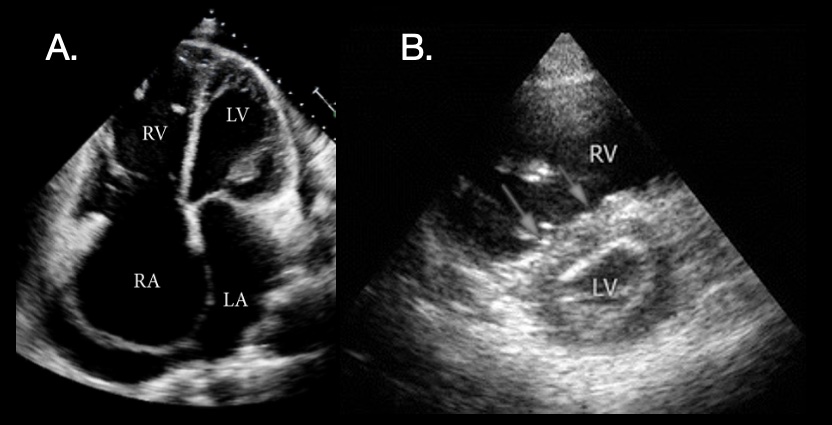
PE POCUS: (A) Significant Right-Sided Distention 1; (B) “D-Sign” on Short-Axis View with Dilated RV, Flattened Septum (Arrows), and D-Shape of LV 2
Pulmonary Ultrasound
A-Lines
- Echogenic Horizontal Lines that Gradually Fade at Equal Intervals from the Pleural Line
- Represents Artifact Reflecting Back and Forth from the Probe and Pleura Due to Air Beneath the Pleura
- Indicates Normal Parenchyma
B-Lines (Lung Comets/Rockets)
- Vertical Artifacts Originating from the Pleural Line
- Due to Increased Density of Lung Parenchyma
- Occasional B-Lines (1-2) Can Be Normal – Particularly in the Lung Bases
- Frequent B-Lines (≥ 3 in a Single-View) Represent Abnormal Tissue
Lung Sliding
- Movement of the Two Pleural Layers During Respiration
- Indicates that the Two Layers are in Apposition
- Represents a Normal Finding
- Absent Lung Sliding Can Be Due to Pneumothorax or Pleural Effusion
- Lung Sliding on M-Mode:
- Seashore Sign: Pleura and Chest Wall Appear as Horizontal Lines (Sea) While Lung Parenchyma Appears as Grainy Sand (Shore)
- Indicates Lung Sliding and Represents Normal Parenchyma
- Barcode (Stratosphere) Sign: Entirely Uniform Horizontal Lines (Resembling a Barcode)
- Indicates a Lack of Underlying Lung Sliding Concerning for Pneumothorax
- Seashore Sign: Pleura and Chest Wall Appear as Horizontal Lines (Sea) While Lung Parenchyma Appears as Grainy Sand (Shore)
- Lung Point: The Interface Between Normal Lung Tissue (With Lung Sliding) and a Pneumothorax (Absent Sliding)
- Used to Evaluate the Size of a Pneumothorax – More Lateral/Posterior Lung Point Indicates a Larger Size
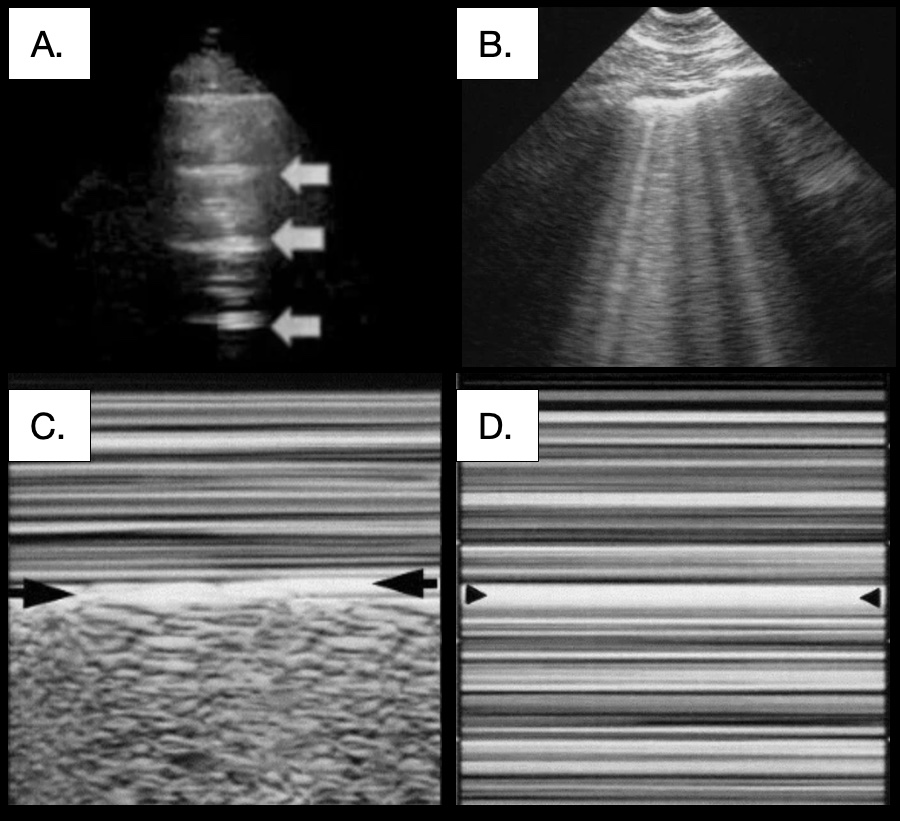 Pulmonary POCUS: (A) A-Lines (Arrows) 5; (B) B-Lines 6; (C) Seashore Sign 6; (D) Barcode Sign 6
Pulmonary POCUS: (A) A-Lines (Arrows) 5; (B) B-Lines 6; (C) Seashore Sign 6; (D) Barcode Sign 6 Inferior Vena Cava (IVC) Ultrasound
Fluid Responsiveness
- POCUS of the IVC is Used to Assess Fluid Responsiveness
- *See Fluid Responsiveness
IVC Diameter
- A Static Measurement of IVC Diameter
- Normal Diameter: 13-17 mm and Not Completely Compressible
- < 13 mm: Unlikely to Be Volume Responsive
- > 25 mm: Likely to Be Volume Responsive
- Generally Poor Accuracy, Although Extreme Values (Flat vs Full) May Be More Predictive
IVC Collapsibility Index (Caval Index)
- Change in IVC Diameter Throughout the Respiratory Cycle in Spontaneously Breathing Patients
- IVC CI (%) = (Max – Min) / Max Diameter
- Maximum Diameter on Expiration
- Minimum Diameter on Inspiration
- Interpretation:
- Near 50-100% Indicatives Fluid Responsiveness
- Near 0% Indicatives Fluid Non-Responsiveness
- Positive Pressure Ventilation is a Contraindication – Positive Pressure on Inspiration Prevents IVC Collapse
IVC Distensibility Index
- Change in IVC Diameter Throughout the Respiratory Cycle in Mechanically Ventilated Patients
- IVC DI (%) = (Max – Min) / Min Diameter
- Maximum Diameter on Inspiration
- Minimum Diameter on Expiration
- Increase ≥ 18% Indicates Fluid Responsiveness
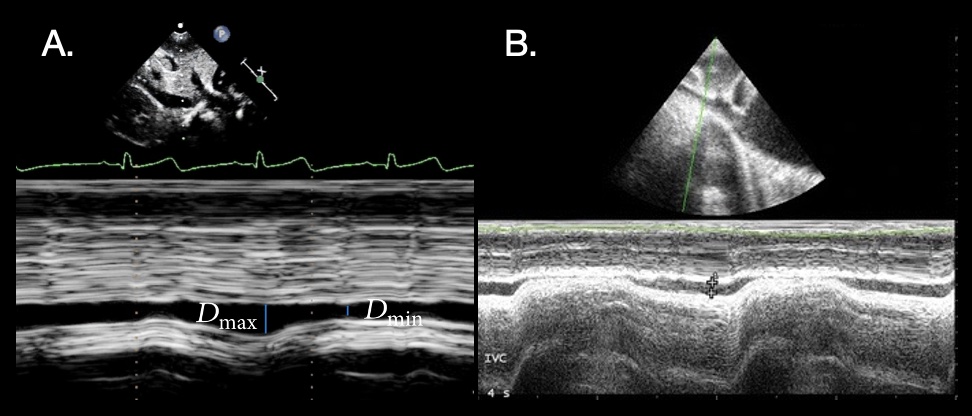
IVC Collapsibility POCUS: (A) Normal 1; (B) Collapse 2
References
- Gaspar HA, Morhy SS. The Role of Focused Echocardiography in Pediatric Intensive Care: A Critical Appraisal. Biomed Res Int. 2015;2015:596451. (License: CC BY-3.0)
- Mok KL. Make it SIMPLE: enhanced shock management by focused cardiac ultrasound. J Intensive Care. 2016 Aug 15;4:51. (License: CC BY-4.0)
- Lakatos B, Tősér Z, Tokodi M, Doronina A, Kosztin A, Muraru D, Badano LP, Kovács A, Merkely B. Quantification of the relative contribution of the different right ventricular wall motion components to right ventricular ejection fraction: the ReVISION method. Cardiovasc Ultrasound. 2017 Mar 27;15(1):8. (License: CC BY-4.0)
- Seif D, Perera P, Mailhot T, Riley D, Mandavia D. Bedside ultrasound in resuscitation and the rapid ultrasound in shock protocol. Crit Care Res Pract. 2012;2012:503254. (License: CC BY-3.0)
- Gargani L, Volpicelli G. How I do it: lung ultrasound. Cardiovasc Ultrasound. 2014 Jul 4;12:25. (License: CC BY-4.0)
- Lichtenstein DA. Lung ultrasound in the critically ill. Ann Intensive Care. 2014 Jan 9;4(1):1. (License: CC BY-2.0)
Cover Photo: Lichtenstein DA, Mauriat P. Lung Ultrasound in the Critically Ill Neonate. Curr Pediatr Rev. 2012 Aug;8(3):217-223. (License: CC BY-2.5)
