Peripheral Vascular Injury
Peripheral Vascular Injury
David Ray Velez, MD
Table of Contents
Background
Peripheral Vascular Injury Can Be Limb and Life Threatening
Etiology
- The Majority are Due to Penetrating Mechanisms – Gunshot Wounds (50%) and Stab Wounds (30%)
- Blunt Vascular Injuries are More Rare (5-25%) but are Associated with Worse Outcomes and Higher Rates of Limb Loss
The Majority of Peripheral Vascular Injuries are in the Lower Extremities
Signs of Vascular Ischemia (6 P’s)
- Pain
- Paresthesia (Pins and Needles Sensation)
- Paresis (Weakness) or Paralysis (Unable to Move)
- Pallor (Pale Color)
- Poikilothermic (Cold)
- Pulseless
AAST Peripheral Vascular Injury Scale
- *See AAST
- Injury Scale is Under Copyright
Ischemia > 3 Hours Can Cause Irreversible Neuromuscular Changes and After 6 Hours There is Myonecrosis and Wallerian Degeneration of Peripheral Nerves
Initial Evaluation and Management
The First Step in Managing Severe Peripheral Vascular Injury is to “Stop the Bleed” (Manual Pressure vs Tourniquet)
Junctional Bleeding (Groin/Axilla) Can Be Particularly Difficult to Control but Options Include Manual Pressure, Wound Packing, Hemostatic Dressings (QuickClot Combat Gauze), or Junctional Tourniquets (If Available)
Major/Hard Signs of Vascular Injury
- Active Arterial Hemorrhage
- Expanding or Pulsatile Hematoma
- Absent Pulse
- Palpable Thrill or Audible Bruit
Minor/Soft Signs of Vascular Injury
- History of Significant Arterial Hemorrhage at the Scene
- Nonexpanding Hematoma
- Diminished Pulse
- Proximity to Major Vessels
- Neurologic Deficit
Initial Management
- Unstable or Major/Hard Signs: Emergent Surgical Exploration
- Stable and Minor/Soft Signs: Imaging (API First; Then CTA if API < 0.9)
Arterial Pressure Index (API)
- Arterial Pressure Index (API) = Arterial Pressure Distal to the Injury / Arterial Pressure of an Uninjured Upper Extremity
- Used for Lower Extremity Injuries
- Arterial Brachial Index (ABI) = Ankle Arterial Pressure Distal to the Injury / Branchial Arterial Pressure
- A Form of API Used for Lower Extremity Injuries
- Brachial Pressure is Taken as the Highest from Either Side
- Uses the Systolic Blood Pressure (SBP)
- Not Reliable in Diabetes or ESRD – Calcified Vessels Give False Elevation
- Measurement Technique:
- Use a Doppler US Over the Distal Artery to Insonate Flow
- Use a Manual Pressure Cuff and Inflate Until the Sound is Lost
- Decrease Pressure Slowly Until the Sound is Heard Again – The Systolic Blood Pressure (SBP)
- *Avoid Using an Automated Blood Pressure Cuff – Less Accurate

Petit Tourniquet from the Civil War

Combat Application Tourniquet (CAT) 1
Surgical Management
Operative Sequence
- Step 1. Temporary Bleeding Control
- Manual Pressure
- Wound Packing
- Hemostatic Dressings (QuickClot Combat Gauze)
- Foley Balloon Catheter Inserted into the Wound if Deep and Narrow
- Tourniquet
- Junctional Tourniquets (If Available)
- Step 2. Extensive Exposure
- Step 3. Definitive Control (Proximal and Distal)
- Step 4. Decision (Definitive Repair vs Damage Control)
Concomitant Orthopedic Injury
- Bony Stabilization Before Vascular Reconstruction
- If Extremity is Grossly Ischemic or Actively Hemorrhaging – Temporarily Control with a Shunt Prior to Bony Stabilization
Vascular Exposure
Prophylactic Fasciotomy Indications
- Ischemia > 6 Hours
- High Risk Injury:
- Combined Arterial/Venous Injury
- Complex Extremity Fractures
- Arterial or Venous Vascular Ligation
- Significant Crush Injury
- *See Fasciotomy
Arterial Injury
< 50% Circumference
- Small Injuries are Generally Managed by Arteriorrhaphy (Primary Repair)
- Complex Injuries May Require Patch Angioplasty if Concerned for Vessel Narrowing/Stricture
> 50% Circumference or Transection
- Injuries > 50% Circumference are Generally Resected and Managed as a Complete Transection
- Short-Segment (< 2 cm): Debride with End-to-End Anastomosis
- Long-Segment (> 2 cm): Bypass or Interposition Graft
- Preferred Graft: Contralateral Saphenous Vein
- Other Graft Options: Ipsilateral Saphenous Vein or PTFE
- *See Great Saphenous Vein (GSV) Harvest
Consider Proximal and Distal Thrombectomy Prior to Closure
Damage Control: Temporary Shunt vs. Ligation
Temporary Vascular Shunts
- Types:
- Improvised Shunts:
- Chest Tubes
- IV Tubing
- Feeding Tubes
- Commercially Available Shunts
- Improvised Shunts:
- Diameter:
- Diameter Should Be Chosen to Best Match the Corresponding Vessel
- Goal: Largest Possible Without Forcing
- Length:
- Commercially Available Shunts Should Generally Not Be Trimmed – Smooth Edges Avoid Intimal Damage
- Improvised Shunts Should Allow At least 2 cm Overlap on Each Side
- Removal:
- Maximum Length of Time Able to Leave in Situ is Unknown
- Perform Definitive Repair as Soon as Feasibly Safe
- Most Remain Patent for 24-48 Hours

Temporary Shunt Past a Femoral Artery Injury 2
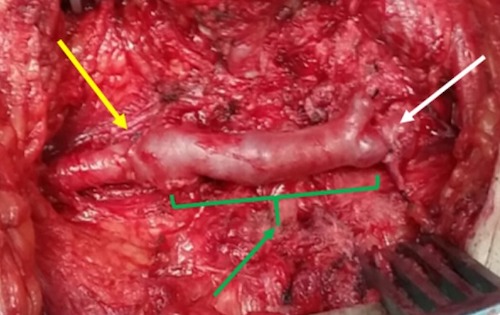
CFA Repair by GSV Interposition Graft 3
Venous Injury
Definition
- Proximal Venous Injury: IVC to Popliteal Veins or SVC to Axillary Veins
- Distal Venous Injury: Distal to the Popliteal or Axillary Veins
Distal Injury is Generally Managed Nonoperatively or by Ligation if Found Intraoperatively
Management of Proximal Injury
- Decision is Made for Surgical Repair vs Ligation Based on Severity of Injury and Hemodynamic Status
- Options for Surgical Repair:
- Lateral Venorrhaphy
- End-to-End Anastomosis
- Patch Venoplasty
- Interposition Graft (Autologous Vein vs Prosthetic Conduit) for Segmental Loss
- Additional Considerations with Ligation:
- Judicious Use of Fasciotomy
- Limb Elevation
- Limb Compression
- Consider Prophylactic Long-Term Anticoagulation Due to DVT/PE Risk – Minimal Data to Guide Use
References
- Indnam. Wikimedia Commons. (License: CC BY-SA-3.0)
- Krüger A, Florido C, Braunisch A, Walther E, Yilmaz TH, Doll D. Penetrating arterial trauma to the limbs: outcome of a modified protocol. World J Emerg Surg. 2013 Dec 4;8(1):51. (License: CC BY-2.0)
- Al-Wahbi AM, Elmoukaied S. Leg ischemia post-varicocelectomy. Int Med Case Rep J. 2016 Mar 8;9:57-60. (License: CC BY-NC-3.0)
