Pelvic Fracture
Pelvic Fracture
David Ray Velez, MD
Table of Contents
Background
Pelvic Fractures are Common After High-Energy Blunt Trauma and Frequently Associated with Multiple Additional Injuries (Mean ISS 18)
Most Common Cause: Motor Vehicle Crash (MVC)
Bimodal Distribution
- Teens/Young Adults – High-Energy Unstable Fractures
- Elderly – Low-Energy Fractures
The Most Feared Complication is Rapid and Uncontrolled Hemorrhage
- Over 1/3 Will Require Transfusion During Their Hospital Stay
Bleeding Source
- Venous Plexus – The Most Common Source (80-90%)
- From Shearing of the Posterior Plexus
- Tends to Be Self-Limited and Hematoma Tamponades
- Fixation Will Also Tamponade Most Venous Bleeding
- Arterial (10-20%)
- Often in Posterior Fractures from Shearing/Compression of the Iliac Vessels Against the Pelvic Brim
- Most Common Artery: Superior Gluteal Artery
- More Likely to be Hemodynamically Unstable
- Cancellous Bone

Open Book Pelvic Fracture 1
Diagnosis
Diagnosis Can Be Made Clinically But is Most Often Made on Imaging (CT is the Gold Standard)
A Normal Physical Exam Can Effectively Rule Out Significant Injury (93-100% Sensitivity) if There are No Distracting Injuries
May Demonstrate External Rotation of the Lower Extremity and Limb-Length Discrepancy
Examination of Pelvic Stability
- Maneuver: Gentle Compression of Iliac Crests Toward the Midline Followed by Divergent Compression/Distraction
- Used to Assess for Pelvic Stability – Stop Immediately if Any Mobility is Felt
- Stop
- Caution: Do Not “Rock” or “Spring” the Pelvis and Only Preform Once – Risk to Worsen Bleeding
- Examination Has Low Sensitivity Itself
Pelvic Fracture Requires a Thorough Examination of the Perineum, Rectum, and Genitalia
Anteroposterior (AP) Plain Film – Often Part of the Primary Survey for Early Detection of Significant Pelvic Disruption
- May Be Omitted in Stable Patients with Low Concern if CT is Being Performed
- Poor Overall Sensitivity (64-78%)
Classification
“Open Book” Fracture: A Colloquial Term to Describe a Fracture with Significant Pelvic Ring Disruption Resembling the Opening of a Book
- Indicates a Combined Anterior and Posterior Injury with High Risk for Vascular Injury
- If Anterior Ring is Widened > 2.5 cm There is Increased Risk of Posterior Injury and Hemorrhage
Multiple Classifications Systems Exist – The Young-Burgess Classification and Tile Classification are the Two Most Common
Young-Burgess Classification
- Anterior-Posterior Compression (APC)
- Type 1: Symphysis Widening < 2.5 cm, Posterior Ligaments Intact
- Type 2: Symphysis Widening > 2.5 cm, Anterior Sacroiliac (SI) Joint Opening/Diastasis, Posterior Sacroiliac (SI) Ligaments Intact
- Type 3: Complete Disruption of the Symphysis and Anterior and Posterior Sacroiliac (SI) Ligaments
- Lateral Compression (LC)
- Type 1: Unilateral Sacral ala Fracture and Pubic Rami Fracture – The Most Common LC Fracture Type
- Type 2: Unilateral Iliac Wing (Crescent) Fracture
- Type 3: Ipsilateral Type 1 or 2 LC Fracture with a Contralateral APC Fracture, “Wind-Swept Pelvis”
- Vertical Shear (VS): Vertical Displacement of the Hemipelvis with Anterior and Posterior Injury
- Combined Mechanism (CM): Combination of Any of the Above
Tile Classification
- Type A – Rotationally and Vertically Stable
- Type A1: Fracture Not Involving the Ring (Avulsion or Iliac Wing)
- Type A2: Minimally Displaced Ring Fracture
- Type A3: Transverse Sacral Fracture
- Type B – Rotationally Unstable, Vertically Stable
- Type B1: Open Book Injury (Due to External Rotational Forces)
- Type B2: Lateral Compression Injury (Due to Internal Rotational Forces)
- Type B3: Bilateral Type B Fractures
- Type C – Rotationally and Vertically Unstable
- Type C1: Vertical Shear Fracture
- Type C2: Ipsilateral Type C1 Fracture with a Contralateral Type B Fracture
- Type C3: Bilateral Type C1 Fractures
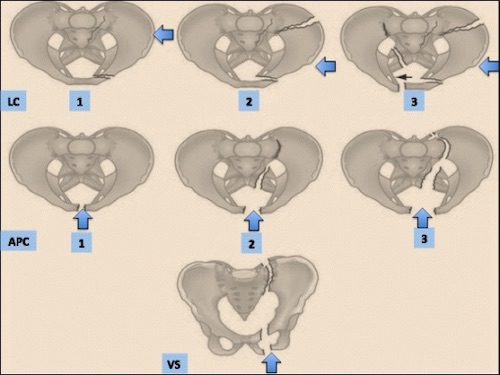
Young and Burgess Classification 2
Treatment
Pelvic Binders
- A Device Placed Around the Pelvis to Compress and Stabilize the Pelvic Ring
- Goal: Reduce Pelvic Volume to Tamponade Venous Bleeding and Limit Fracture Motion
- Multiple Commercially Available Devices are Used but Can Use a Bed Sheet and Penetrating Towel Clamps if Not Readily Available
- The Binder Should Be Snug but Not Overtight – Centered at the Level of the Greater Trochanter
- Often Mistakenly Placed Too High (Around the Iliac Crests) Which Can Cause Excessive Abdominal Pressure Without Pelvic Stabilization
- Consider a Repeat AP Plain Film After Placement to Confirm Appropriate Reduction
- Can Compromise Skin and Create Pressure Injuries if Left Too Long
- *Theoretically, Binders Can Worsen Displacement of Lateral Compression (LC) Fractures and Worsen Bleeding – Some Recommend Against Binders in These Situations Although There is No Clinical Evidence of Significant Harm
Hemodynamically Unstable Patients with a Positive FAST Should Undergo Emergent Exploratory Laparotomy
Hemorrhage Control
- The First Step in Hemorrhage Control is Generally a Pelvic Binder for Temporary Pelvic Stabilization
- Angioembolization
- Often the Preferred Method for Definitive Hemorrhage Control if Readily Available
- Complications: Impotence or Pelvic/Gluteal Ischemia
- Proceed with External Fixation to Tamponade Venous Bleeding if There Continues to Be Evidence of Bleeding After Embolization
- Preperitoneal Pelvic Packing (PPP)
- *See Preperitoneal Pelvic Packing (PPP)
- Some Prefer Over Angioembolization – Particularly if Time to Angioembolization is Delayed
- PPP Has Decreased Crude Mortality Compared to Angioembolization – However, Studies are Heterogenous with Significant Differences in Populations and Unable to Make a Conclusive Comparison
- 27% of Patients Treated with PPP Did Not Achieve Adequate Hemorrhage Control and Still Required Subsequent Angioembolization
- *PPP is Contraindicated as the Initial Intervention if Hemodynamically Unstable and FAST is Positive – Requires Laparotomy
- Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA)
- Placed into Zone III for Pelvic Hemorrhage
- Laparotomy
- Generally Not a Good Option for Pelvic Hemorrhage
- Often Difficult to Visualize and Can Restart Bleeding
- May Consider Laparotomy Followed by PPP if Laparotomy is Required with Concomitant Pelvic Hemorrhage – Attempt to Keep Incisions Separate
Control of Bleeding from an Open Fracture Includes Packing Through the Laceration and Pelvic Binder, Followed by Angioembolization and External Fixation
Fracture Management
- Stable Pelvic Ring: Conservative Management and Weight Bear as Tolerated
- Includes: LC-I, APC-I, and Isolated Pubic Rami Fractures
- Unstable Pelvic Ring: Surgical Repair
- Angioembolization Should Be Performed First if Indicated – Pelvic Binder Serves Same Purpose as Surgical Fixation Until Hemorrhage Can Be Temporized
- May Consider Temporary External Fixation (Ex-Fix) Until More Stable and Appropriate for Definitive Fixation

Pelvic Binder 3

Pelvic Binder (Before and After) 4

Preperitoneal Pelvic Packing 5
References
- Finnan RP, Herbenick MA, Prayson MJ, McCarthy MC. Bladder incarceration following anterior external fixation of a traumatic pubic symphysis diastasis treated with immediate open reduction and internal fixation. Patient Saf Surg. 2008 Oct 19;2(1):26. (License: CC BY-2.0)
- Coccolini F, Stahel PF, Montori G, Biffl W, Horer TM, Catena F, Kluger Y, Moore EE, Peitzman AB, Ivatury R, Coimbra R, Fraga GP, Pereira B, Rizoli S, Kirkpatrick A, Leppaniemi A, Manfredi R, Magnone S, Chiara O, Solaini L, Ceresoli M, Allievi N, Arvieux C, Velmahos G, Balogh Z, Naidoo N, Weber D, Abu-Zidan F, Sartelli M, Ansaloni L. Pelvic trauma: WSES classification and guidelines. World J Emerg Surg. 2017 Jan 18;12:5. (License: CC BY-4.0)
- Vaidya R, Roth M, Zarling B, Zhang S, Walsh C, Macsuga J, Swartz J. Application of Circumferential Compression Device (Binder) in Pelvic Injuries: Room for Improvement. West J Emerg Med. 2016 Nov;17(6):766-774. (License: CC BY-4.0)
- Vaidya R, Roth M, Zarling B, Zhang S, Walsh C, Macsuga J, Swartz J. Application of Circumferential Compression Device (Binder) in Pelvic Injuries: Room for Improvement. West J Emerg Med. 2016 Nov;17(6):766-774. (License: CC BY-4.0)
- Jang JY, Shim H, Jung PY, Kim S, Bae KS. Preperitoneal pelvic packing in patients with hemodynamic instability due to severe pelvic fracture: early experience in a Korean trauma center. Scand J Trauma Resusc Emerg Med. 2016 Jan 13;24:3. (License: CC BY-4.0)
