PEG Tube
Percutaneous Endoscopic Gastrostomy (PEG)
David Ray Velez, MD
Table of Contents
Indications
General Considerations
- Gastrostomy Tube Is Placed Through the Skin with Endoscopic Guidance/Assistance
- Requires Both a Surgeon and Endoscopist
- Generally Done AFTER a Tracheostomy if Done Simultaneously
- Problems with Prolonged Nasogastric (NG) Tube:
- More Complications (Nasal Irritation, Ulceration, Bleeding, Reflux, and Aspiration)
- Increased Discomfort
- Lower Feeding Efficacy
- Similar Morbidity and Mortality to Surgical Gastrostomy Tube
Indications
- Generally Indicated if at Risk for Moderate-Severe Malnutrition within 2-3 Weeks of Nasogastric Tube Feeding
- Neurologic Disease:
- Traumatic Brain Injury (TBI)
- Cerebrovascular Accident (CVA)/Stroke
- Dementia
- Parkinson’s Disease
- Multiple Sclerosis (MS)
- Amyotrophic Lateral Sclerosis (ALS)
- Cerebral Palsy
- Cerebral Tumors
- Hypoxic Ischemic Encephalopathy
- Reduced Level of Consciousness
- Prolonged Coma
- Cancer:
- Palliative Gastric Decompression for Chronic Bowel Obstruction or Ileus
- Abdominal Malignancy
- Head and Neck Cancer
- Facial Surgery
- Esophageal Cancer
- Gastrointestinal (GI) Disease:
- Tracheoesophageal Fistula (TEF)
- Enterocutaneous Fistula (ECF)
- Cystic Fibrosis
- Short Bowel Syndrome
- Crohn’s Disease
- Other Possible Indications:
- Trauma
- Severe Burn Wounds
- Wasting Syndrome in HIV/AIDS
- Intensive Care Patients
Contraindications
- Absolute Contraindications:
- Massive Ascites
- Unable to Pass Endoscope into Stomach
- Interposed Organs (Liver or Colon)
- Hemodynamic Instability
- Sepsis
- Uncorrectable Coagulopathy
- Abdominal Wall Infection at Access Site
- Past Total Gastrectomy
- If Being Used for Feeding: Severe Gastroparesis or Gastric Outlet Obstruction
- Relative Contraindications:
- Esophageal Cancer (Compromise Future Gastric Conduit)
- Hepatosplenomegaly
- Peritoneal Dialysis
- Portal Hypertension with Gastric Varices
- Past Partial Gastrectomy
Classic “Pull” Technique
Start with Endoscopy into the Stomach
- Ensure No Anatomic Obstacles
- Insufflate the Stomach
Gain Access Through Abdominal Wall by a Safe Technique
- Transillumination: Externally Visualize Light from the Endoscope Through the Abdominal Wall at the Chosen Site
- Should Be About 2 cm Below Costal Margin
- Finger Indentation: Endoscopically Visualize Gastric Wall Indentation When Digital Pressure is Applied with 1:1 Motion
- Needle Access: A Needle with Saline Syringe Under Negative Pressure is Inserted Through the Abdominal Wall into the Gastric Lumen
- Stool or Air Bubbles Before Entering the Stomach Indicates Inadvertent Bowel Entry
- OK to Retry if See Air Bubbles First
Pull Looped Wire Through the Mouth
- A Snare is Placed Through the Endoscope and Looped Around the Needle
- A Soft Looped Wire is Inserted Through the Needle and Then Grabbed with the Snare
- The Endoscope is Removed While Maintaining a Hold on the Wire
- Pulls the Wire through the Mouth
- The Distal End Will Still Protrude from the Abdominal Wall
Pull PEG Tube Through the Abdominal Wall
- The Wire Loop from the Mouth is then Secured to the PEG Tube
- The Wire is Then Pulled Back Through the Abdominal Wall, Pulling the PEG Tube with It
- The Needle is Removed Once the Tube Hits the Gastric Wall
- The PEG Tube is then Pulled Through the Abdominal Wall Until the Internal Bolster Rests Along the Gastric Wall
- Caution When Pulling to Not Pull the Entire PEG Through the Abdominal Wall
- Endoscope is Reinserted to Confirm Position
- Can Potentially Grasp the Internal Bolster with the Endoscopic Snare Before Pulling the PEG Through to Ease Reentry by Pulling the Endoscope Along with the PEG
Place the External Bolster and Cut the Tube to Size
- Bolster Should Lie 1-2 cm from the Skin
- Snug but Not Too Tight (Will Necrose Stomach Wall)
PEG (Introducer Technique) 1
Other Techniques
“Push” Technique (Sachs-Vine)
- Initial Access is Similar to the “Pull” Technique
- Pull a Guidewire Through the Mouth Instead of a Looped Wire
- PEG Tube is Then Pushed Down Through the Mouth Over the Guidewire
- Once Seen Emerging the Tube is Then Pulled Through the Abdominal Wall
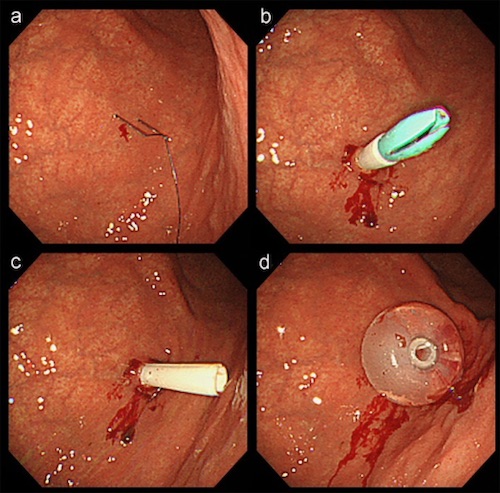
“Introducer Technique” (Russel)
- Endoscope is Used Only to Insufflate and Observe
- Initial Access is Similar to the “Pull” Technique
- A Guidewire Placed Through Needle and the Needle is Removed
- An Introducer with an Outer Sheath is Passed Over the Guidewire and Then the Sheath and Introducer are Removed
- The PEG Tube (Balloon Deflated) is Passed Through Sheath
- Sheath Then Pulled Away
- The Balloon is Inflated and the PEG Tube is Appropriately Secured
Complications
Similar Morbidity and Mortality to Surgical Gastrostomy
Procedural Complications
- Aspiration
- Hemorrhage
- Perforation of Viscera
- Ileus
Infection
- Overall Risk: 30% – The Most Common Complication
- The Majority are Minor and Require No Intervention
- Risk Factors:
- Diabetes
- Obesity
- Malnutrition
- Steroid Therapy
- Excessive Pressure from the Bolster on the Skin
- Reduced Risk by Giving Prophylactic Antibiotics Prior to the Procedure
- Treatment: Antibiotics
- Minor Infections Can Be Managed with 5-7 Days of Oral Antibiotics
- Major or Systemic Infections Require IV Antibiotics
- Necrotizing Soft Tissue Infections are Rare but Require Immediate Aggressive Surgical Intervention
Dislodged Tube/Inadvertent Removal
- Risk: 1.6-4.4%
- Most Common Cause: Excessive Traction in Combative or Confused Patients
- Initial Management: Replace at Bedside and Confirm Placement by XR with Water-Soluble Contrast Through the Tube
- If Replacement Fails: OR for Replacement (Emergent if < 2 Weeks – Tract Not Yet Formed)
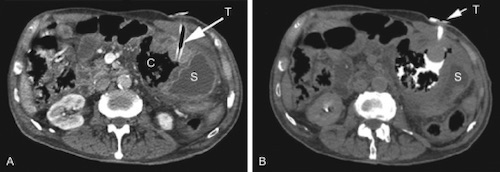
PEG Dislodged; Contrast Extravasation 2
Buried Bumper Syndrome
- Partial or Complete Overgrowth of Gastric Mucosa Over the Internal Bolster
- Risk: 0.3-2.4%
- Internal Bolster Can Migrate Through the Gastric Wall and Lodge Along the Tract
- Risk Factors:
- Malnutrition
- Poor Wound Healing
- Excessive Tension Between the Bolsters
- Presentation:
- Peristomal Leakage
- Infection
- Abdominal Pain
- Resistance to Formula Infusion
- Diagnosis: Endoscopy or CT Scan
- Treatment: Remove the PEG and Replace
Peristomal Leakage
- Risk: 1-2%
- Largest Risk Factors:
- Malnutrition
- Diabetes
- Poor Wound Healing
- Should Prompt Examination for Infection, Ulceration, or Buried Bumper
- If Tract is Mature (> 4 Weeks) You Can Remove the Tube for 24-48 Hours to Allow the Tract to Close Slightly Before Replacing
Tube Obstruction
- Tubes Often Clog with Tube Feeds or Medications
- Prevention:
- All Medications Should be Either Liquid Form of Dissolved in Liquid
- Always Flush with ≥ 20-30 cc Saline/Water After Feeds or Medications
- Never Use Bulking Agents Through the Tube
- Management: Flush with 60 cc Saline/Warm Water
- Other Fluid Options: Pancreatic Enzymes or Specialized Gastrostomy Brush
Gastrocolocutaneous Fistula
- Caused During the Initial Placement by the PEG Penetrating Through Interposed Colon Before the Stomach
- Often Recognized After Removal and Replacement of the Original Tube
- Presentation:
- Sudden Onset Diarrhea – From Tube Feeds Entering the Transverse Colon
- Feculent Material in the PEG Tube
- Feculent Vomiting – From Retrograde Passage into the Stomach
- Diagnosis: Upper GI Study – Shows Contrast Passage from the Stomach into the Colon
- Treatment: Removal of Feeding Tube to Allow Tract Healing
- Laparotomy if Peritonitis or Signs of Leak
References
- Toh Yoon EW, Kobayashi M. Percutaneous Endoscopic Gastrostomy in a Patient With Continuous Intrathecal Baclofen Infusion Therapy. Gastroenterology Res. 2017 Apr;10(2):132-134. (License: CC BY-NC-4.0)
- Soares da Silva MQ, Lederman A, Coelho da Rocha RF, Lourenção RM. Feeding tube replacement: not always that simple! Autops Case Rep. 2015 Mar 30;5(1):49-52. (License: CC BY-NC-3.0)
