Pulmonary Embolism (PE)
Pulmonary Embolism (PE)
David Ray Velez, MD
Table of Contents
Definition
Pulmonary Embolism (PE): Blood Clot Occlusion of the Pulmonary Arteries, Most Often Due to a DVT
Classification
- High-Risk (Massive) Pulmonary Embolism: Obstructive Shock or Hypotension
- Intermediate-Risk (Submassive) Pulmonary Embolism: Right Ventricle (RV) Dysfunction or Myocardial Ischemia (MI) but No Shock/Hypotension
- Intermediate-High Risk: Both Right Ventricle (RV) Dysfunction AND Myocardial Ischemia (MI)
- Intermediate-Low Risk: Either Right Ventricle (RV) Dysfunction OR Myocardial Ischemia (MI)
- Low-Risk (Non-Massive) Pulmonary Embolism: No Right Ventricle (RV) Dysfunction, Myocardial Ischemia, or Shock/Hypotension
Location
- Saddle Pulmonary Embolism: A Large PE Sitting in the Bifurcation of the Pulmonary Artery Where it Splits into the Right and Left Lungs
- High Mortality Risk
- Segmental Pulmonary Embolism: Affects the 3rd Division of the Pulmonary Arteries – The Initial Branches Off the Lobar Arteries
- Subsegmental Pulmonary Embolism (SSPE): Affects the 4th Division of the Pulmonary Arteries
Physiology
Most Common Source: Iliofemoral DVT
Pathophysiology
- Mechanisms of Impaired Gas Exchange:
- Ventilation-Perfusion (V:Q) Mismatch Due to Increased Dead Space from Mechanical Obstruction
- Functional Intrapulmonary Shunting from Inflammation Causing Surfactant Dysfunction and Atelectasis
- Impaired Gas Exchange Causes Hypoxia
- Hypoxia Causes Tachycardia and Tachypnea
- Tachypnea Leads to Hypocapnia and Respiratory Alkalosis
Risk for Sudden Cardiac Arrest and Circulatory Collapse
30% Mortality if Untreated
Presentation
Many are Asymptomatic
Presentation
- Dyspnea – Most Common Symptom
- Pleuritic Chest Pain
- Cough
- Wheezing
- Hemoptysis
- Anxiety
Physical Exam
- Tachypnea
- Tachycardia
- Hypotension
- Fever
- Pale Skin
May Also Have Signs/Symptoms of DVT
- Swelling
- Pain
- Warmth
- Erythema
Diagnosis
Wells Score
- Used to Predict the Probability of PE Based on History and Physical Exam
- Factors:
- Physical Findings of DVT – 3 Points
- No Better Alternative Diagnosis – 3 Points
- Tachycardia (HR > 100) – 1.5 Points
- Immobilization (≥ 3 Days) or Recent Surgery (< 4 Weeks) – 1.5 Points
- History of DVT/PE – 1.5 Points
- Hemoptysis – 1 Point
- Malignancy – 1 Point
- “Traditional” Wells Interpretation:
- > 6: High Probability
- 2-5: Moderate Probability
- 0-1: Low Probability
- “Modified” Wells Interpretation:
- > 4: PE Likely
- ≤ 4: PE Unlikely
D-Dimer
- Not Often Used in Surgical Practice
- Highly Sensitive but Not Specific
- D-Dimer < 500 ng/mL Likely Excludes the Diagnosis of PE
- If Low-Moderate Probability of PE: Consider D-Dimer Prior to Imaging
- Can Possibly Avoid CT if D-Dimer is Low
Arterial Blood Gas (ABG) Findings
- Hypoxemia
- Respiratory Alkalosis
- Widened Alveolar-Arterial Oxygen Gradient
EKG Findings
- Tachycardia – Most Common EKG Finding
- S1Q3T3 Pattern (Indicates Right Ventricle Strain) – Rarely Seen
- T1-4 Inversion
Echocardiography Findings
- Left Ventricle (LV): Normal Function
- Right Ventricle (RV): Severely Dilated with Reduced Systolic Function/Wall Hypokinesis
- Septal Flattening (From RV Pressure Overload)
- Pulmonary Artery Hypertension
- McConnell Sign– RV Dysfunction with Akinesia of the Mid-Free Wall but Normal Motion at the Apex
- Highly Specific for PE
- D-Sign– Left Ventricle is “D” Shaped Due to Flattening of the Interventricular Septum from Right Ventricular Overload
Definitive Diagnosis
- Definitive Diagnosis is Based Primarily on Imaging
- CT Pulmonary Angiogram
- Gold Standard Diagnostic Test
- Ventilation-Perfusion Scan
- Often Used in Women of Child-Bearing Age – Less Breast Radiation (However Has More Fetal Radiation if Pregnant)
- If Unstable & High Clinical Probability: Empirically Treat Before Definitive Diagnosis
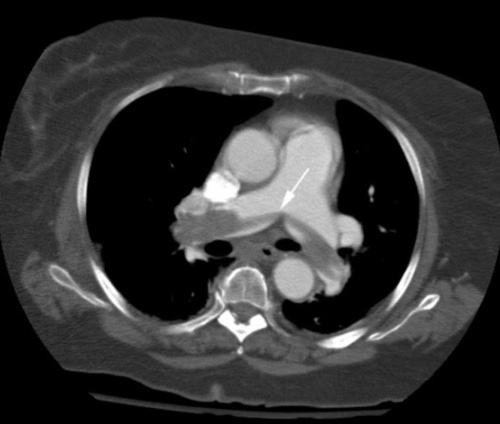
Saddle Pulmonary Embolism on CTA 1
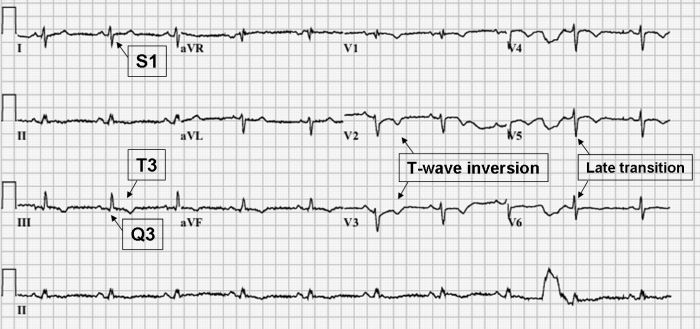
S1Q3T3 on EKG 2
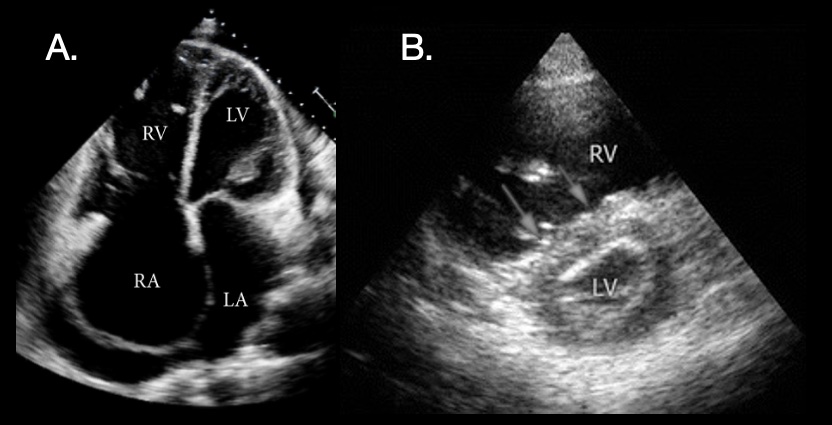
PE POCUS: (A) Significant Right-Sided Distention; (B) “D-Sign” on Short-Axis View with Dilated RV, Flattened Septum (Arrows), and D-Shape of LV 3,4
Pulmonary Embolism Severity Index (PESI)
Used to Predict the 30-Day Morbidity and Mortality for Patients with Diagnosed Pulmonary Embolism
Factors
- Demographics:
- Age: +1 Point per Year
- Male Sex: +10 Points
- Comorbid Illness:
- Cancer: +30 Points
- Heart Failure: +10 Points
- Chronic Lung Disease: +10 Points
- Clinical Findings:
- Altered Mental Status: +60 Points
- Systolic Blood Pressure (SBP) < 100 mmHg: +30 Points
- Heart Rate ≥ 110 bpm: +20 Points
- Respiratory Rate (RR) ≥ 30 bpm: +20 Points
- Temperature < 36°C: +20 Points
- Arterial O2 Saturation < 90%: +20 Points
Class/Mortality
| PESI Score | Class | 30-Day Mortality |
| 0-65 | I | 0.0-1.6% |
| 66-85 | II | 1.7-3.5% |
| 86-105 | III | 3.2-7.1% |
| 106-125 | IV | 4.0-11.4% |
| > 125 | V | 10-24.5% |
Treatment
Hemodynamically Unstable: Systemic Thrombolytics
- Consider Catheter-Directed Thrombolysis if High Bleeding Risk
- Right Ventricular Strain Alone Does Not Require Thrombolysis if Stable
- May Require Surgical Embolectomy if Thrombolysis is Contraindicated or Fails
Hemodynamically Stable: Anticoagulation
- Generally Initiated on a Heparin Drip
- 80 U/kg Bolus with 18 U/Kg/Hr Infusion
- Goal PTT: 60-90
- Avoid Intubation if Able – Does Not Resolve Hypoxia and May Cause Hemodynamic Collapse
May Consider Outpatient Treatment for Low-Risk Patients with PESI Class I-II in the Right Clinical Setting – Outside the Scope of Critical Care
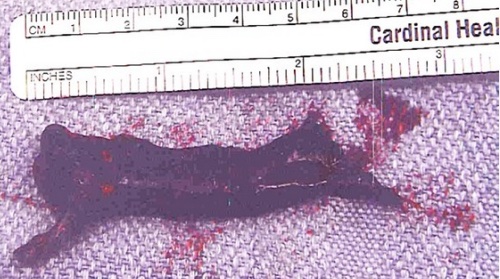
Pulmonary Embolism Removed by Thrombectomy 5
References
- Lee K, Rincon F. Pulmonary complications in patients with severe brain injury. Crit Care Res Pract. 2012;2012:207247. (License: CC BY-3.0)
- Todd K, Simpson CS, Redfearn DP, Abdollah H, Baranchuk A. ECG for the diagnosis of pulmonary embolism when conventional imaging cannot be utilized: a case report and review of the literature. Indian Pacing Electrophysiol J. 2009 Sep 1;9(5):268-75. (License: CC BY-2.5)
- Gaspar HA, Morhy SS. The Role of Focused Echocardiography in Pediatric Intensive Care: A Critical Appraisal. Biomed Res Int. 2015;2015:596451. (License: CC BY-3.0)
- Mok KL. Make it SIMPLE: enhanced shock management by focused cardiac ultrasound. J Intensive Care. 2016 Aug 15;4:51. (License: CC BY-4.0)
- Bhargava M, Dincer E. Traveling thrombus in the right atrium: is it the final destination? Case Rep Pulmonol. 2012;2012:378282. (License: CC BY-3.0)
