Necrotizing Soft Tissue Infection (NSTI)
Necrotizing Soft Tissue Infection (NSTI)
David Ray Velez, MD
Table of Contents
Definitions
Necrotizing Soft Tissue Infection (NSTI): Necrotizing Infection of the Skin and Soft Tissue
Necrotizing Cellulitis: NSTI of the Skin (Sparing Fascia and Deep Muscle Compartments)
Necrotizing Fasciitis: NSTI of the Fascia
- Spreads Along Fascia Deep to the Subcutaneous Tissue
- Poor Blood Supply Along the Fascial Planes Allows More Rapid Spread of Bacteria Before Skin Changes are Seen
Necrotizing Myositis: (Non-Clostridial) NSTI Extending to the Deep Muscle Compartments
Clostridial Myonecrosis (Gas Gangrene): Clostridial NSTI Extending to the Deep Muscle Compartments
Fournier’s Gangrene: NSTI of the Perineum

Fulminant NSTI of the Arm 1

Fournier’s Gangrene 2
Classification and Microbiology
Classification
- Clostridial Infection
- Non-Clostridial Infection
Clostridial Infection
- Clostridium perfringens – Most Common in Traumatic Gas Gangrene
- Clostridium septicum – Most Common in Non-Traumatic Gas Gangrene
- *Note: Often Associated with Underlying Malignancy
- *Usually Associated with Myonecrosis
Non-Clostridial Infection
- Type I: Polymicrobial – Most Common (75%)
- Type II: Monomicrobial
- Group A Streptococcus – Most Common Monomicrobial Organism
- Staphylococcus aureus (MSSA and MRSA)
- Type III: Marine Bacteria (Vibrio)
- Type IV: Fungal (Candida)
Risk Factors
Risk Factors
- Trauma
- IV Drug Abuse
- Surgery
- Obesity
- Alcoholism
- Immunosuppression (Diabetes, Cirrhosis, HIV)
- Mucosal Brach (Hemorrhoids, Rectal Fissure)
- Malignancy
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) – Debated Association
Diagnosis
Presentation
- Severe Pain (Out-of-Proportion)
- Cellulitis and Erythema (Without Sharp Margins)
- Deeper Infections May Not Have Superficial Cellulitis
- Edema
- Bullae or Ecchymosis
- Visible Skin Necrosis
- Crepitus – From Anaerobic Production of Nitrogen and Hydrogen, Not Readily Absorbed by Tissue
- Hypoesthesia (Decreased Sensation) – Late Finding from Small Blood Vessel Thrombosis and Superficial Nerve Destruction
- Fever
- Murky Gray (“Dishwater”) Fluid Drainage
Diagnosis
- Diagnosis is Clinical and Only Confirmed by Surgical Exploration
- Radiology Findings: Soft Tissue Gas, Fluid Collections, and Inflammatory Change
- CT Scan is the Best Initial Imaging
- Labs:
- Elevated WBC and CRP
- Decreased Sodium
- Elevated Creatinine (AKI)
- Hyperglycemia
Laboratory Risk Indicator for Necrotizing Fasciitis (LRINEC) Score
- Interpretation/Chance of NSTI:
- Low Risk (0-5 Points): < 50%
- Intermediate Risk (6-7 Points): 50-75%
- High Risk (8-13 Points): > 75%
- *Specific but Poor Sensitivity – Should Not Be Used to Rule Out
- *Note: CRP ≥ 150 Has the Strongest Predictive Value (+4)
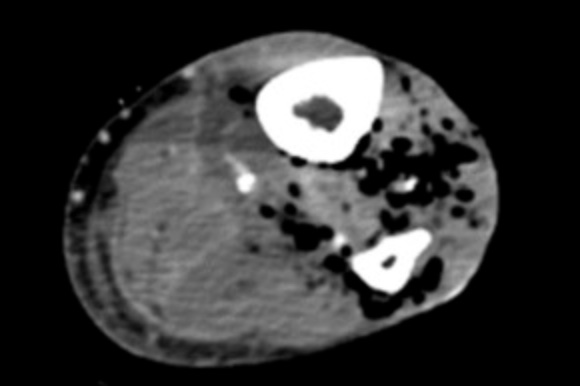
Soft Tissue Gas on CT 3

Soft Tissue Gas on XR
| CRP | WBC | Hgb | Na | Cr | Glu | |
| 0 | < 150 | < 15 | > 13.5 | ≥ 135 | ≤ 1.6 | ≤ 180 |
| +1 | 15-25 | 11-13.5 | > 180 | |||
| +2 | > 25 | < 11 | < 135 | > 1.6 | ||
| +4 | ≥ 150 |
Treatment
Primary Management: Emergent Aggressive Surgical Debridement and Broad-Spectrum Antibiotics
- Rapidly Progresses with High Mortality (25%)
Surgical Debridement
- Aggressive Surgical Debridement Emergently
- Serial Wet-to-Dry Dressing Changes (May Consider Using Dakin’s Solution)
- May Require Repeat Debridement Every 1-2 Days
- Can Cause Significant Disfigurement and Disability
- Extremities May Require Amputation
Empiric Antibiotics
- Empiric Antibiotic Regimen: Piperacillin-Tazobactam or Carbapenem Plus Vancomycin and Clindamycin
- Broad-Spectrum Coverage:
- Piperacillin-Tazobactam (Zosyn)
- Meropenem (Merrem)
- Ertapenem (Invanz)
- Imipenem
- MRSA Coverage:
- Vancomycin – Most Common
- Daptomycin – Not for Pneumonia (Inactivated by Lung Surfactant)
- Linezolid – Not for Bacteremia or Endocarditis
- Clindamycin
- Use to Inhibit Ribosomal Exotoxin Synthesis
- Reduces the Production of Panton-Valentine Leucocidin (PVL) in Staphylococcus aureus
- *Deescalate Based on Intraoperative Cultures
Adjunct Therapies
- Hyperbaric Oxygen Therapy (HBOT)
- May Have Reduced Morbidity and Mortality but Controversial and Data is Not Clear
- Not Readily Availability at Most Institutions
- Intravenous Immunoglobulin (IVIG)
- May Consider IVIG for Group A Streptococcus (S. pyogenes) to Bind Exotoxin if Not Responding to Other Measures – Based Largely on Management of Toxic Shock Syndrome
- Plasmapheresis
- Diverting Colostomy
- Consider for Severe Perineal Infections
- *Controversial Use
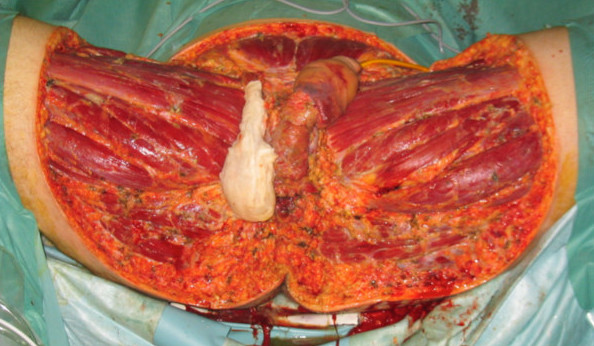
Aggressive Surgical Debridement 4
References
- Adigun IA, Nasir AA, Aderibigbe AB. Fulminant necrotizing fasciitis following the use of herbal concoction: a case report. J Med Case Rep. 2010 Oct 19;4:326. (License: CC BY-2.0)
- Heiner JD, Eng KD, Bialowas TA, Devita D. Fournier’s Gangrene due to Masturbation in an Otherwise Healthy Male. Case Rep Emerg Med. 2012;2012:154025. (License: CC BY-3.0)
- Spadaro S, Berselli A, Marangoni E, Romanello A, Colamussi MV, Ragazzi R, Zardi S, Volta CA. Aeromonas sobria necrotizing fasciitis and sepsis in an immunocompromised patient: a case report and review of the literature. J Med Case Rep. 2014 Sep 22;8:315. (License: CC BY-4.0)
- Meyer Ganz O, Gumener R, Gervaz P, Schwartz J, Pittet-Cuénod B. Management of unusual genital lymphedema complication after Fournier’s gangrene: a case report. BMC Surg. 2012 Dec 23;12:26. (License: CC BY-2.0)