Neck Trauma
Neck Trauma
David Ray Velez, MD
Table of Contents
Zone Management
Zones of the Neck
- Zone I: Thoracic Inlet to Cricoid Cartilage
- Zone II: Cricoid Cartilage to Angle of Mandible
- Most Commonly Injured Zone
- Zone III: Angle of Mandible to Base of Skull
“Hard Signs” of Injury – Definitive Indications of Arterial/Structural Injury
- Active Hemorrhage
- Expanding or Pulsatile Hematoma
- Bruit or Thrill
- Subcutaneous Emphysema or Air Bubbling from Wound
“Soft Signs” of Injury – Possible Indications of Arterial/Structural Injury
- Dysphagia
- Dysphonia or Voice Changes
- Hemoptysis
- Nonexpanding Hematoma
Initial Management
- Stable and No Hard Signs: CTA
- Historically All Zone II Injuries Required Surgical Exploration
- May Consider Observation Alone if Stable and Asymptomatic with No Hard or Soft Signs
- Unstable or Hard Signs: Surgical Exploration
Gaining Vascular Control at Surgery
- Approach:
- Incision is Made Along the Anterior Border of the Sternocleidomastoid Muscle (SCM) – Similar to a Carotid Endarterectomy
- If Bilateral Exploration is Required – Can Make Bilateral Incisions that Connect Inferiorly in a “U”-Shape
- Zone I: Proximal Control Requires Median Sternotomy
- Zone II: Direct Control
- Zone III: Distal Control Requires Mandible Disarticulation vs Antegrade Embolectomy Catheter
- Generally Considered the Most Challenging
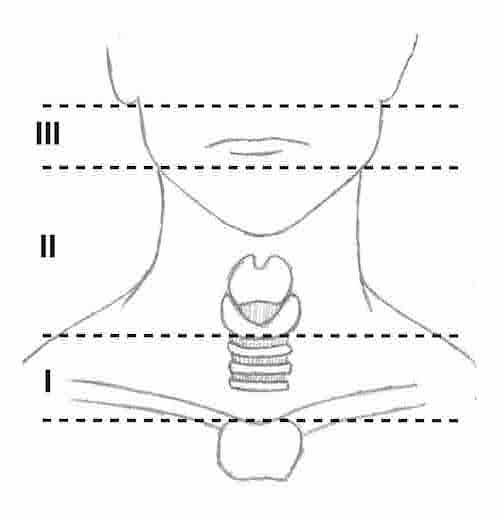
Zones of the Neck
Vascular Injury
Blunt Cerebrovascular Injury (BCVI)
Penetrating Arterial Injury
- Internal Carotid Artery (ICA) Injury:
- Options for Surgical Repair:
- Primary Arteriorrhaphy
- Patch Angioplasty
- End-to-End Anastomosis
- Vein or PTFE Graft
- ECA Transposition to Injured ICA
- Ligation Indications:
- Hemodynamically Unstable
- Very Severe Neck Injury
- Zone III ICA Injury at the Skull Base
- High Risk for Stroke/CVA if Ligated (75-80%)
- Options for Surgical Repair:
- External Carotid Artery (ECA) Injury:
- May Attempt to Repair if Stable and Controlled
- Safe to Ligate if Needed
Venous Injury
- Generally Ligate Small Veins without Concern
- Internal Jugular (IJ) Vein: Transverse Venorrhaphy if Able
- Safe to Ligate if Necessary for Major Hemorrhage or Hemodynamic Instability
Tracheoesophageal Injury
Larynx/Trachea Injury
- Most Common in Penetrating Trauma
- Symptoms:
- Neck Pain
- Dysphagia
- Dyspnea
- Cough or Hemoptysis
- Subcutaneous Emphysema
- Air Bubbling from Wound
- Pneumothorax (PTX)
- Vocal Cord Paralysis
- Diagnosis: Laryngoscopy/Bronchoscopy
- Treatment of Small Injuries: Repair Transversely in 1-Layer with Absorbable Suture
- 2-Layer Repairs Risk Stenosis
- Include Tracheal Rings in the Repair
- Treatment of Large Injuries: Primary Anastomosis
- Can Generally Perform Primary Anastomosis for Injuries Up to 5-6 Tracheal Rings in Length with Mobilization
- Strongly Consider Tracheostomy – Place in Standard Position or Possibly Through the Injured Site
- Consider Reinforcement with a Vascularized Pedicle or Intercostal or Strap Muscles
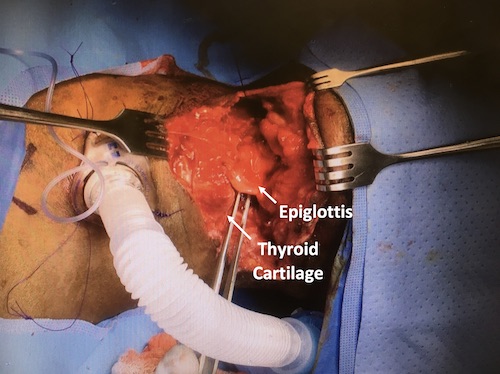
Larynx Laceration
Esophagus Injury
- Hardest Cervical Injury to Identify
- Most Common in Penetrating Trauma
- Most Common Site: Cervical #1, Thoracic #2, and Abdominal #3
- Diagnosis:
- Able to Swallow: Water-Soluble Esophagram
- If Negative but High-Suspicion: Dilute-Barium Esophagram
- If Still Negative: Esophagoscopy
- *Contrast Studies Have High False-Negative Rates (25%)
- Intubated or Unable to Swallow: Esophagoscopy
- Able to Swallow: Water-Soluble Esophagram
- Primary Treatment: Surgical Repair, Buttress, and Leave a Drain
- First Extend the Myotomy to See the Full Length of Mucosal Injury
- Close in Two Layers: Inner Absorbable, Outer Permanent
- Strength Layer: Submucosa (No Serosa in the Esophagus)
- Buttress in the Neck: Strap Muscles or SCM
- Devastating Injury (Repair Not Immediately Feasible): Cervical Esophagostomy (Spit Fistula)
