Myocardial Infarction (MI)
Myocardial Infarction (MI)
David Ray Velez, MD
Table of Contents
Definitions
Basics
- Coronary Artery Disease is the Most Common Cause of Death in the United States
- 95% of Myocardial Ischemia is Due to Underlying Atherosclerotic CAD
- Most Atherosclerosis is Proximal
- Risk Factors for Increased Mortality:
- Cardiogenic Shock – Strongest Risk Factor
- Emergency Setting
- Increased Age
- Low Ejection Fraction
Definitions
- Acute Coronary Syndrome (ACS): A Constellation of Clinical Symptoms Consistent with Acute Myocardial Ischemia
- Includes Myocardial Infarction (MI) and Unstable Angina (UA)
- Coronary Artery Disease (CAD): Diseased/Damaged Coronary Blood Vessels
- Angina Pectoris: Severe Chest Pain Due to Inadequate Cardiac Blood Supply
- Myocardial Infarction (MI/Heart Attack): Death of Myocardial Cells Due to Obstruction of Blood Flow
Types of Angina Pectoris
- Stable Angina: Brief Episodes Associated with Exercise or Stress and Relieved with Rest
- Unstable Angina (UA)
- Prolonged Angina at Rest (> 20 Minutes)
- New-Onset Severe Angina
- Worsening Angina (More Frequent, Severe, or Longer Duration)
- Variant/Prinzmetal Angina: Angina Due to Coronary Artery Spasm
Types of Myocardial Infarction (MI)
- ST-Segment Elevation Myocardial Infarction (STEMI): MI Associated with an ST-Segment Elevation
- Indicates a Full-Thickness Injury
- Non-ST-Segment Elevation Myocardial Infarction (NSTEMI): MI Not Associated with an ST-Segment Elevation
- Indicates a Subendocardial (Not Full-Thickness) Injury
- Type 1 NSTEMI – Spontaneous from Atherothrombotic Plaque Rupture or Erosion
- Type 2 NSTEMI – Due to Oxygen Supply-Demand Imbalance
- Type 3 NSTEMI – Cardiac Death without Biomarker Samples or Detected at Autopsy
- Type 4 NSTEMI – Associated with Revascularization Procedures
- 4a: Related to Percutaneous Coronary Intervention (PCI) within 48 Hours
- 4b: Related to Stent Thrombosis
- 4c: Restenosis After Percutaneous Coronary Intervention (PCI)
- Type 5 NSTEMI – Related to CABG Procedure within 48 Hours
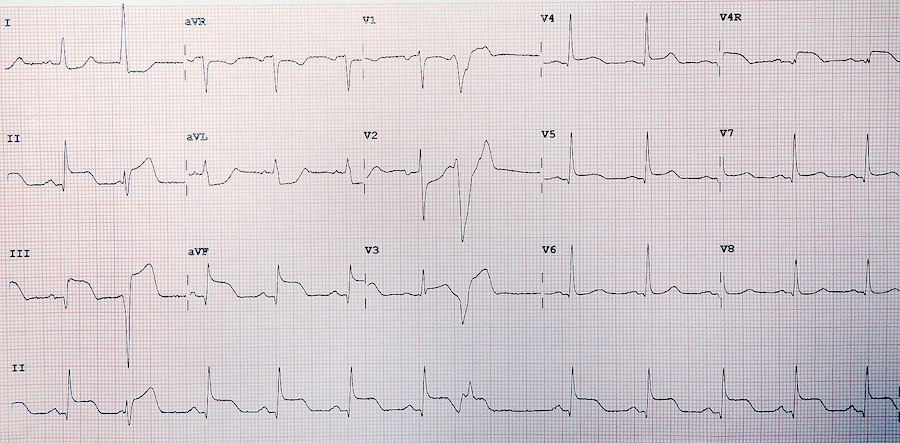
STEMI on EKG
Diagnosis
Presentation
- Chest Pain/Discomfort – Most Common Symptom
- Classic Description: Substernal Chest Tightness/Pressure with Radiation to Left Arm or Jaw
- “Feels like an Elephant Standing on My Chest”
- Shortness of Breath
- Diaphoresis
- Weakness
- Anxiety
Diagnosis of Myocardial Infarction (MI)
- Elevated Troponin with ≥ One Of:
- Symptoms of Myocardial Ischemia
- New Ischemic Changes on EKG
- Development of Pathologic Q Waves
- New Loss of Viable Myocardium or Regional Wall Motion Abnormality Consistent with Ischemic Etiology on Imaging
- Identification of a Coronary Thrombus by Angiography or Autopsy
- Coronary Angiogram is the Standard Tool for Describing Surgical Anatomy of CAD
Differentiation
- STEMI: Elevated Troponin with ST-Elevation on EKG
- NSTEMI: Elevated Troponin without ST-Elevation on EKG
- UA: Normal Troponin
EKG Changes
- ST-Segment Changes (Elevation or Depression)
- Left Bundle Branch Block (LBBB)
- T Wave Inversion
- Q Waves
- Lead Laterality:
- Anterior: V1-V4 (Indicates Left Anterior Descending (LAD) Artery Disease)
- Posterior: V1 and V2 (Indicates Right Coronary Artery or Left Circumflex Artery Disease)
- Lateral: I and aVL (Indicates Left Circumflex Artery Disease)
- Inferior: II, III, and aVF (Indicates Right Coronary Artery Disease)
Cardiac Enzymes
- Troponin I
- Best Test for Detecting Acute MI
- Highest Sensitivity and Specificity
- Remains Elevated for 5-14 Days
- Generally Trended Every 3-6 Hours
- Creatine Kinase-MB (CK-MB)
- Remains Elevated for 2-3 Days
- Best for Detecting Recurrence
Treatment
Cardiogenic Shock
Medical Managements
- Oxygen Supplementation
- Antiplatelet Therapy (Aspirin or Clopidogrel (Plavix))
- Other NSAIDs Should Be Discontinued – Increased Risk of Cardiovascular Events
- Beta Blockers
- Contraindicated in Heart Failure, Heart Block, or Cardiogenic Shock
- HMG-CoA Reductase Inhibitor (Statin)
- Sublingual Nitroglycerin – Vasodilation to Relieve Chest Pain
- Contraindicated in Hypotension or Cardiogenic Shock
- Consider Morphine for Persistent Severe Pain
Reperfusion
- STEMI Requires Early Reperfusion – The Most Important Factor in Improving Survival
- Options:
- Percutaneous Coronary Intervention (PCI)
- Preferred Approach if a Cath Lab is Immediately Available
- Goal Door-to-Balloon Time < 90 Minutes
- Fibrinolysis
- Coronary Artery Bypass Graft (CABG)
- Percutaneous Coronary Intervention (PCI)
Percutaneous Coronary Intervention (PCI)
- PCI Generally Refers to Coronary Angioplasty with Stent Placement
- Radial Access is Generally Preferred Over Femoral Access (Decreased Risk of Bleeding Complications)
- Stent Types:
- Drug-Eluting Stents (DES)
- Polymer Coating with Compounds Used to Decrease the Risk of Restenosis
- Generally Preferred but Require Longer Anticoagulation
- Bare Metal Stent (BMS)
- Drug-Eluting Stents (DES)
- Dual Antiplatelet Therapy (DAPT)
- Most Common Agents: Aspirin and Clopidogrel (Plavix)
- Duration of Therapy:
- Drug-Eluting Stents (DES): One Year
- Bare Metal Stent (BMS): One Month
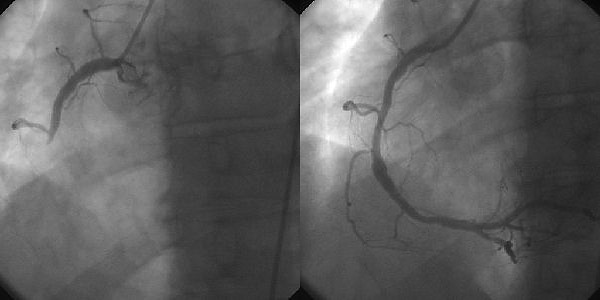
PCI: Before (Left) and After (Right) 1
Coronary Artery Bypass Graft (CABG) Indications
- Left Main Disease > 50% Stenosis
- Triple-Vessel Disease > 70% Stenosis (RCA, LAD, and Circumflex)
- Double-Vessel Disease Including the Proximal LAD
- At Least One Vessel with Significant (> 70%) Stenosis and Unacceptable Angina Despite Medical Therapy
- Survivors of Sudden Cardiac Death with Ischemia-Mediated Ventricular Tachycardia
- Undergoing Noncoronary Cardiac Surgery with Left Main Disease (> 50%) or Any Other CAD (> 70%)
- Emergency CABG:
- After Failed Percutaneous Coronary Intervention (PCI) with Ongoing Ischemia or Threatened Occlusion of Substantial Myocardium
- Cardiogenic Shock Due to Myocardial Infarction (MI)
Complications
Mechanical Complications After Acute MI
- 3 Classic Presentations:
- Papillary Muscle Rupture– Causes Severe Mitral Regurgitation with Fulminant Heart Failure and Pulmonary Edema
- Posteromedial Papillary Muscle Rupture is Most Common Due to Singular Blood Supply (RCA/Inferior MI)
- Interventricular Septum Rupture– Causes a Left-to-Right Shunt with Pulmonary Vascular Congestion
- Left Ventricular Free Wall Rupture– Causes a Pericardial Effusion and Tamponade
- Papillary Muscle Rupture– Causes Severe Mitral Regurgitation with Fulminant Heart Failure and Pulmonary Edema
- Generally Present Around 3-5 Days After an MI
- High Level of Concern for Patients that Become Acutely Hypotensive After an MI (High Mortality)
- Temporization:
- Afterload Reduction (Diuresis or Vasodilators) for Papillary Muscle or IV Septum Rupture
- Fluids to Increase Preload for LV Wall Rupture
- Usually Require Emergent Surgical Repair
Post-Cardiac Injury Syndrome (PCIS)
- Also Known As:
- Dressler’s Syndrome
- Post-Pericardiotomy Syndrome
- Post-Myocardial Infarction Syndrome
- Definition: Pericarditis from Injury to the Pericardium
- Develops Weeks-Months After Myocardial Infarction (MI)
- Presentation:
- Pericardial Friction Rub
- Fever
- Pleuritic Chest Pain
- Shortness of Breath
- Can Cause Pericardial Effusion
- EKG Findings: Diffuse ST-Segment Elevation
- Treatment: NSAIDs, Colchicine, and Steroids
Other Complications
- Reinfarction
- Generally Occurs Within 48 Hours
- Postinfarct Angina
- Conduction Abnormalities
- Left Ventricular Aneurysm
References
- JHeuser. Wikimedia Commons. (License: CC BY-SA-3.0)
