Liver Trauma
Liver Trauma
David Ray Velez, MD
Table of Contents
Anatomy
Background
Initial Evaluation and Management
Nonoperative Management (NOM)
Surgical Management
– Exposure and Hemostasis
– Definitive Management
If trauma surgery is a contact sport, the badly injured liver is the Ninja Master: a vicious, cunning and lethal adversary. – “Top Knife” by Hirshberg & Mattox
Anatomy
Couinaud Segments
- Anatomical Divisions – Each Has Own Vascular Inflow, Outflow, and Biliary Drainage
- Caudate Lobe
- Segment I – Entire Caudate Lobe
- Left Lobe
- Segment II – Superior Left Lateral
- Segment III – Inferior Left Lateral
- Segment IVa – Superior Left Medial
- Segment IVb – Inferior Left Medial (Quadrate)
- Right Lobe
- Segment V – Inferior Right Anteromedial
- Segment VI – Inferior Right Posterolateral
- Segment VII – Superior Right Posterolateral
- Segment VIII – Superior Right Anteromedial
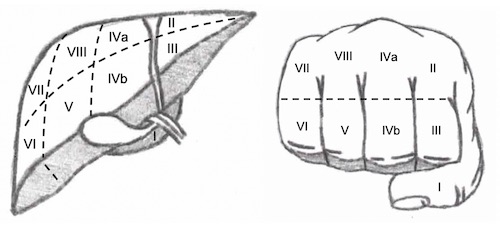
“Handy” Mnemonic of Couinaud Segments
Vasculature
- Arterial System (Supplies 25%)
- Proper Hepatic Artery Branches into the Left and Right Hepatic Arteries
- Middle Hepatic Artery Branches off the Left
- The Biliary System Depends on the Arterial Supply
- Portal System (Supplies 75%)
- Venous Drainage
- Segment I Drains Directly into the IVC
- Left Hepatic Vein – Drains Segments II and III into the IVC
- Middle Hepatic Vein – Drains Segments IVA/B, V, and VIII into the Left Hepatic Vein
- Right Hepatic Vein – Drains Segments V-VIII into the IVC
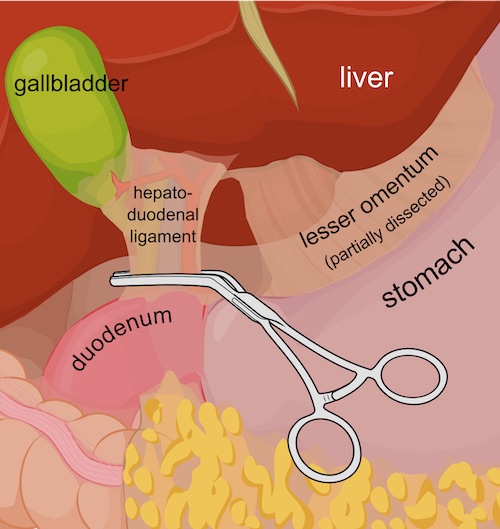
Structures
- Porta Hepatis/Portal Fissure – Transverse Fissure Between Caudate (I) and Quadrate Lobes (IVb) on the Visceral Surface
- Cantlie’s Line – Imaginary Division Separating the Left and Right Lobes
- From Gallbladder Fossa to Middle Hepatic Vein/IVC
- Portal Triad
- Contains the Bile Duct (Lateral), Proper Hepatic Artery (Medial), and Portal Vein (Posterior)
- Contained within Hepatoduodenal Ligament
- Enters Porta Hepatis
- Ligaments
- Falciform Ligament – Separates the Medial and Lateral Left Lobe
- Attaches to Anterior Abdominal Wall/Umbilicus
- Contains the Ligamentum Teres
- Ligamentum Teres (Round Ligament) – Carries Remnant Umbilical Vein
- Contained in the Free Edge of the Falciform Ligament
- Ligamentum Venosum – Remnant Ductus Venosus
- From the Ligamentum Teres to the IVC
- Falciform Ligament – Separates the Medial and Lateral Left Lobe
Background
Etiology
- The Most Commonly Injured Intraabdominal Organ Overall
- Blunt Abdominal Trauma:
- Second Most Common Organ Injury in Blunt Abdominal Trauma (35-45%)
- *Remains Controversial and Reports Vary Between Spleen and Liver
- Penetrating Abdominal Trauma:
- Third Most Common Organ Injury in Penetrating Abdominal Trauma (30%), Behind Small Bowel and Colon
- *Some Older Texts Report Liver as the Most Common Injury in Penetrating Abdominal Trauma
AAST Liver Injury Scale (2018 Revision)
- *See AAST
- Injury Scale is Under Copyright
Liver Trauma 1
Initial Evaluation and Management
Unstable: Laparotomy
- First Perform a FAST (Focused Assessment with Sonography in Trauma) to Confirm Abdominal Source
- Diagnostic Peritoneal Lavage (DPL) is Rarely Performed but May Be Considered if FAST is Inconclusive
- Search for Oher Sources if Negative
- Diffuse Peritonitis Indicates Bowel Injury and Warrants Laparotomy – Diffuse Peritonitis Should Never be Attributed to Solid Organ Injury as Isolated Hemoperitoneum Should Not Cause Diffuse Peritoneal Irritation
Stable: CT Imaging
Indications for Angiography and Embolization (93% Success Rate)
- Transient Responder
- Active Extravasation (“Blush”) – Controversial as There is Some Evidence that Stable Patients with Contrast Extravasation Can Initially Be Managed by Observation Without Angioembolization (Similar Rates of Liver-Related Complications and Mortality)
- Pseudoaneurysm
- Arteriovenous Fistula (AVF)
Stable Patients Generally Undergo a Trial of Nonoperative Management (With or Without Angioembolization) Unless There are Other Indications for Surgery
Surgery Solely for Washout of Blood is Generally Not Indicated Unless for Severe Refractory Pain
Nonoperative Management (NOM)
The Exact Definitions for Nonoperative Management are Poorly Defined
Admission
- Consider ICU Admission for 24-72 Hours for Injuries ≥ Grade III
- Consider an Initial NPO Status for up to 24 Hours if Closely Monitoring
- Exact Hospital Length of Stay is Poorly Defined
Activity Restrictions
- Bedrest: Consider for 24-48 Hours
- Previously Defined as Injury Grade + One Day (1999 APSA Guidelines)
- Activity Restriction: Return to Unrestricted Activity at Injury Grade + 2 Weeks
- Defined as “Normal” Age-Appropriate Activities
- Longer Restrictions for Contact Sports (Football, Wrestling, Hockey, etc.) – Less Well Defined but Often Range from 2-6 Months
Indications for Surgery (After a Trial of Nonoperative Management)
- Angioembolization Failure
- Hemodynamic Instability
- Persistent Bleeding
- Refractory Abdominal Pain
- *May Consider Angiography and Embolization if Stable and Not Already Attempted
Start DVT Prophylaxis Early (Within 24-48 Hours) for Solid Organ Injury if Otherwise Clinically Appropriate
Repeat CTA – Controversial
- Routine Use without Clinical Indication is Not Useful
- Most Studies Show that Routine Use is Not Necessary and Rarely Changes Clinical Management
- Some Advocated for Repeat CTA After 2-7 Days, Before Discharge, to Evaluate for Pseudoaneurysm or Arteriovenous Malformation
Surgical Management – Exposure and Hemostasis
Exposure
- Divide the Falciform Ligament – Visualize the Superior or Lateral Aspects
- Divide the Triangular Ligaments – Further Mobilize the Right and Left Lobes
- If a Stable Hematoma is Noted Within the Triangular Ligament: Do Not Enter (Concern for Hepatic Vein or IVC Injury)
Initial Hemostasis
- Manual Compression and Packing Until Resuscitated
- Most Liver Bleeding is Venous
- Pringle Maneuver – If Compression Fails
- Maneuver: Compress the Portal Triad Manually or with a Vascular Clamp
- 85% Success in Complex Injuries
- Can Tolerate Up to 75 Minutes Without Adverse Sequelae
- Failure Raises Concern for Hepatic Vein/IVC Injury
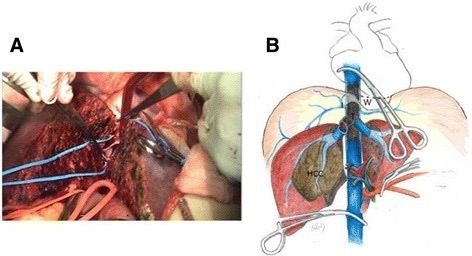
- Total Hepatic Isolation – If All Other Measures Fail
- Components:
- Pringle Maneuver
- Infrahepatic IVC Occlusion
- Suprahepatic IVC Occlusion
- Also Consider Supraceliac Aortic Occlusion – Abdominal Blood Flow Will Be Lost from Circulation Above the Diaphragm
- Components:
- Atriocaval (Schrock) Shunt – Shunt from IVC to Right Atrium to Bypass the Liver
- Considered for Retrohepatic Venous Injury but Rarely Used in Modern Practice
Atriocaval (Schrock) Shunt – Technique
- Pringle Maneuver
- Median Sternotomy
- Prepare a Shunt
- Chest Tube – Cut a Hole 20 cm from the Nearest Drainage Hole
- Endotracheal Tube – Cut a Hole 17-18 cm from the Nearest Hole Past the Balloon
- Control Perihepatic IVC with Rumel Tourniquets:
- Control Suprarenal (Infrahepatic) IVC – Omit Step if Using an ETT
- Control Intrapericardial (Suprahepatic) IVC
- Insert the Shunt Through a Right Atrial Incision
- Apply a Partially Occluding Clamp on the Right Atrial Appendage
- Place a Purse-String Suture
- Create an Incision Between the Purse-String
- Remove the Clamp
- Insert the Shunt Through the Incision and into the IVC
- Palpate the Tube Terminating in the Correct Infrarenal Position
- All Shunt Holes Should Be Outside the Area of Vascular Isolation
- Secure All Site
- Infrahepatic IVC – Either Secure the Rumel Tourniquet or Inflate the ETT Balloon
- Suprahepatic IVC – Secure the Rumel Tourniquet
- Right Atrium – Secure the Purse String
- Shunt End – Clamp the Exposed End of the Shunt Protruding from the Right Atrium
Pringle Maneuver 2
Total Hepatic Isolation 3
Surgical Management – Definitive Management
Minor Injuries (Grade I-II)
- Start with Simple Techniques:
- Manual Compression (5-10 Minutes)
- Topical Agents (Fibrin Glue/Surgicel)
- Electrocautery
- Argon Beam Electrocoagulation
- Secondary Options:
- Superficial Laceration: Suture Hepatorrhaphy (Primary Repair)
- Deep Laceration: Omental Packing and Loosely Approximate Edges
- Liver Suture: Absorbable (0 Chromic) and Blunt Tipped Needle
- Small Suture Can Tear Glisson’s Capsule & Worsen Bleeding
- Tapered/Cutting Needles Can Cause Damage to Vascular or Biliary Structures
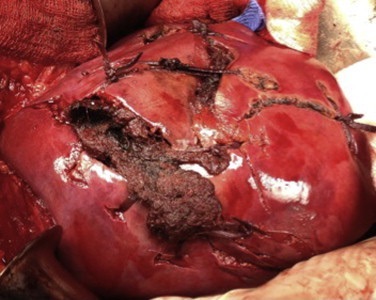
Complex Injuries (Grade III-V)
- Complex Injuries May Require Hepatectomy
- Finger Fracture Technique
- Glisson’s Capsule is Incised Towards the Injury
- Parenchyma is Fractured Between Thumb and Forefinger
- Technique Rapidly Exposes Lacerated Vessels and Bile Ducts for Direct Ligation/Repair
- Debride Devascularized Tissue Once Hemostasis is Achieved
- Consider Omental Pedicle Packing
Juxtahepatic Venous Injury (Grade V)
- Start with Perihepatic Packing
- Options if Continues to Bleed:
- Endovascular Stent When Stable, Before Packing Removal
- Direct Hepatectomy to Reach Injury and Repair
- Venovenous Bypass with Vascular Exclusion and Primary Repair
- Last Resort: Total Hepatectomy and Delayed Liver Transplant
Damage Control: Perihepatic Packing and Planned Reexploration
References
- Latifi R, Khalaf H. Selective vascular isolation of the liver as part of initial damage control for grade 5 liver injuries: Shouldn’t we use it more frequently? Int J Surg Case Rep. 2015;6C:292-5. (License: CC BY-NC-SA-3.0)
- Remesz O. Wikimedia Commons. (License: CC BY-SA-3.0)
- Ho MH, Chen TW, Ou KW, Yu JC, Hsieh CB. Rescue strategy for advanced liver malignancy with retrohepatic inferior vena cava thrombi: experience to promote surgical oncological benefit. World J Surg Oncol. 2017 Apr 12;15(1):83. (License: CC BY-4.0)
