Kidney Trauma
Kidney (Renal) Trauma
David Ray Velez, MD
Table of Contents
Background
Anatomy
- Gerota’s Fascia: Surrounds the Kidney and Perirenal Fat
- Renal Hilum:
- Structures (Anterior-to-Posterior): Vein > Artery > Pelvis
- MNEMONIC: “VAP”
- Renal Artery:
- Right Renal Artery – Travels Posterior to the IVC
- Left Renal Artery – Shorter
- *About 25% Receive Accessory Branches Directly from the Aorta
- Renal Vein:
- Right Renal Vein – Shorter, without Collaterals
- Left Renal Vein – Travels Anterior to the Aorta with Multiple Collaterals
- Branches: Gonadal Vein, Adrenal Vein, and Second Lumbar Vein
The Majority (80-90%) are from Blunt Abdominal Trauma
AAST Kidney Injury Scale (2018 Revision)
- *See AAST
- Injury Scale is Under Copyright
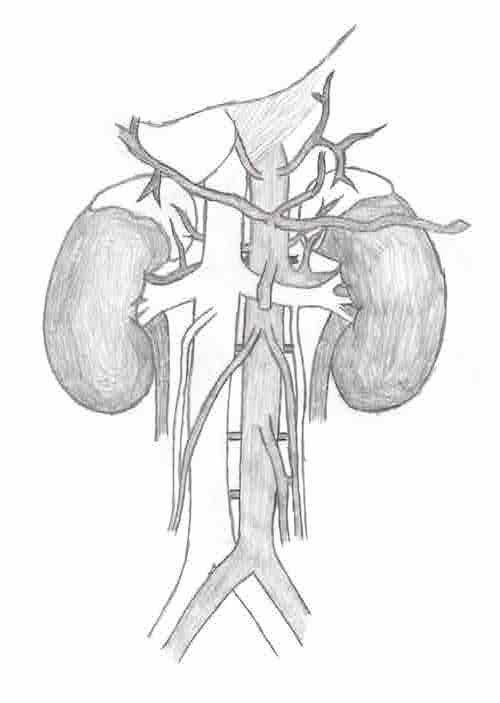
Renal Vasculature
Diagnosis
May Be Diagnosed Intraoperatively or on Radiographic Imaging
Unstable: Laparotomy
- First Perform a FAST (Focused Assessment with Sonography in Trauma) to Confirm Abdominal Source
- Diagnostic Peritoneal Lavage (DPL) is Rarely Performed but May Be Considered if FAST is Inconclusive
- Search for Oher Sources if Negative
- Consider Intraoperative IV Pyelogram (IVP)
- Historically the Standard Approach for Radiographic Diagnosis but Rarely Used in Modern Practice with the Advent of CT
- Accuracy is Variable and May Miss Significant Injuries
- Diffuse Peritonitis Indicates Bowel Injury and Warrants Laparotomy – Diffuse Peritonitis Should Never be Attributed to Solid Organ Injury
Stable: CT Imaging
- The Gold Standard in Modern Diagnostic Imaging
- Obtain Delayed/Excretory Phase Images to Evaluate for Collecting System/Ureter Injury that May Be Missed on Early/Vascular Phase Images Alone
Treatment
The Majority of Renal Injuries are Managed Nonoperatively if Hemodynamically Stable
Indications for Renal Surgical Exploration
- Hemodynamic Instability
- Active Hemorrhage Requiring Massive Transfusion
- Renovascular Pedicle Avulsion
- Ureteropelvic Junction (UPJ) Avulsion
- Pulsatile or Expanding Hematoma (Seen Intraoperatively)
- High-Grade Injury – Debated
- Nonoperative Management Has Higher Rates of Renal Salvage
- Surgical Management Can Offer Earlier Definitive Control and Minimize Risk of Urinoma/Bleeding
Indications for Angiography and Embolization
- Transient Responder
- Active Extravasation (“Blush”)
- Pseudoaneurysm
- Arteriovenous Fistula (AVF)
Parenchymal Injury
- Superficial Laceration: Primary Repair
- Deep Injuries: Debridement vs. Partial Nephrectomy
- Partial Nephrectomy is Done by Sharp Guillotine Transection of a Polar Lesion with Closure of Transected Vessels/Collecting System and Capsule Closure Over the Defect (If Able)
- Nephrectomy May Be Required for Damage Control if Bleeding is Uncontrolled from High-Grade Injury
Renovascular Pedicle Injury
- Active Extravasation/Pseudoaneurysm on CT: Angioembolization
- Active Bleeding at Laparotomy:
- Primary Repair Preferred
- May Need to Ligate Segmental Branches – Results in Distal Ischemia, But Preferred Over Nephrectomy
- Nephrectomy May Be Required for Damage Control
- Renal Artery Occlusion/Devascularization:
- Unilateral (Two Normal Kidneys) – Conservative vs Endovascular Management
- Unilateral (Solitary Kidney) or Bilateral – Surgical Revascularization
- *Left Renal Vein Can Be Ligated Distally (Close to IVC) Due to High Collaterals
- Right Renal Vein is Too Short and Lacks Collaterals
- Maximum Clamp (Warm Ischemia) Time: 20-30 Minutes
Urinary Collecting System Injury
- Urinary Leak: Nonoperative Management
- Consider Stent or Nephrostomy if Fails
- Ureteropelvic Junction (UPJ) Avulsion: Surgical Repair
- Always Use Absorbable Monofilament Suture (Avoid Stricture/Stones)
Renal Exposure
- Consider Exposure and Control of the Renal Pedicle Prior to Renal Exploration – May Decrease Nephrectomy Rates
- Enter the Retroperitoneum by Ipsilateral Medial Visceral Rotation by Mobilizing the Ipsilateral Colon/Mesocolon After Incising the Peritoneal Reflection/Line of Toldt
- Expose the Kidney Through a Vertical Incision Over the Anterior Surface of Gerota’s Fascia
Nonoperative Management (NOM)
The Exact Definitions for Nonoperative Management are Poorly Defined
Admission
- Consider ICU Admission for 24-72 Hours for Injuries ≥ Grade III
- Consider an Initial NPO Status for up to 24 Hours if Closely Monitoring
- Exact Hospital Length of Stay is Poorly Defined
Activity Restrictions
- Bed Rest for 24-72 Hours or Until Gross Hematuria Resolves for Significant Injuries
- Return to Normal Activity After 2-3 Months
Start DVT Prophylaxis Early (Within 24-48 Hours) for Solid Organ Injury if Otherwise Clinically Appropriate
For Grade IV/V Injuries: Repeat CTA After 2-7 Days to Look for Pseudoaneurysm, Arteriovenous Malformation, Urinary Extravasation, or Urinoma
- Early Diagnosis Allows Prompt Treatment Before Development of Associated Complications
- Routine CTA is Less Controversial than with Other Solid Organ Injuries (Liver/Spleen)
