Intracranial Pressure (ICP)
Intracranial Pressure (ICP)
David Ray Velez, MD
Table of Contents
Definition
Intracranial Pressure (ICP): The Pressure within the Skull that the Brain, Blood, and Cerebrospinal Fluid Exert on the Skull’s Dural Envelope
Cerebral Prefusion Pressure (CPP): The Pressure that Drives Blood into the Brain to Deliver Oxygen and Nutrients
- CPP = MAP – ICP
Monro-Kellie Doctrine
- The Sum of the Volumes of the Brain Matter, Cerebrospinal Fluid (CSF), and Intracranial Blood is Constant
- An Increase in One Component Will Cause a Decrease in One or Both of the Others
- Therefore an Elevated ICP will Result in Decreased Cerebral Perfusion Pressure and Risk for Herniation
Normal Values
- Intracranial Pressure (ICP)
- Normal: 7-15 mmHg
- General Goal: < 20 mmHg
- Peaks 48-72 Hours After Trauma
- Cerebral Perfusion Pressure (CPP)
- General Goal: > 60 mmHg to Avoid Secondary Brain Injury
- Range 50-70 mmHg
Signs of Elevation
Cushing’s Triad
- A Triad of Findings Seen from Increased Intracranial Pressure
- Due to Increased Sympathetic and Parasympathetic Activity
- Findings are a Late Sign and Suggest Impending Herniation
- Triad:
- Hypertension (Widened Pulse Pressure)
- Bradycardia
- Irregular Breathing Pattern
- Stages:
- First Stage
- Increased ICP Causes Increased Sympathetic Activity
- Elevated Blood Pressure and Heart Rate
- Second Stage
- Hypertension Activates Aortic Arch Baroreceptors Causing Increased Parasympathetic Activity
- Decreases Heart Rate
- Third Stage
- High ICP, Heart Rate Changes, and Endogenous Stimuli All Distort Brainstem Pressures
- Causes Irregular Breathing
- First Stage
Additional Signs of Elevated ICP
- Pain and Headache
- Double Vision (Due to Cranial Nerve VI Palsy)
- Signs of Uncal Herniation
- Eye Findings are the Earliest Sign of Uncal Herniation
- Ptosis
- Anisocoria (Unequal Pupil Size)
- Impaired Movement
- A Dilated/Blown Pupil Indicates Pressure on Ipsilateral Oculomotor CN III
- Eye Findings are the Earliest Sign of Uncal Herniation
Monitoring
Types of ICP Monitors
- Bolt (Codman/Camino ICP Monitor)
- Bolt Placed into the Parenchyma with Fiberoptic Monitoring
- Only Measures ICP
- External Ventricular Drain (EVD/Ventriculostomy)
- Drain Placed into the Ventricle
- Measures ICP and Allows Therapeutic CSF Drainage
Indications for ICP Monitoring (Bolt vs EVD)
- Severe Head Injury (GCS ≤ 8) with an Abnormal CT
- Severe Head Injury (GCS ≤ 8) with a Normal CT but ≥ 2 of:
- Age > 40
- Motor Posturing
- SBP < 90 mmHg
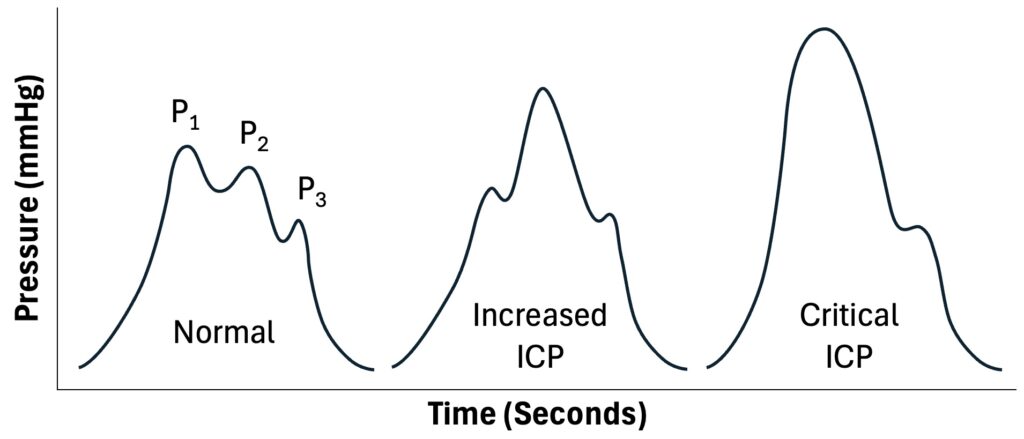
ICP Waveform
- Waveform Peaks:
- P1: “Percussion Wave” – Represents Blood Pressure Transferred to the CSF
- P2: “Tidal Wave” – Represents the Reflection of the Pressure Wave in the Cerebral Parenchyma
- P3: “Dicortic Wave” – Related to Aortic Valve Closure and Venous Pulsation
- Reported Mean ICP Describes the Average of the ICP Peaks Over a Short Period of Time
- Elevated P1 May Represent Hypertension
- Decreased P1 May Represent Loss of CPP
- Elevated P2 May Represent Increased ICP and Decreased Compliance
Optic Nerve Sheath Diameter (ONSD)
- Ultrasound Measurement of the ONSD Allows a Noninvasive Evaluation of ICP
- Elevated ICP is transmitted Through the Subarachnoid Space Increasing the Size of the Optic Nerve Sheath
- ONSD > 5 mm Suggests Elevated ICP
- High Sensitivity (94%) and Specificity (90%)
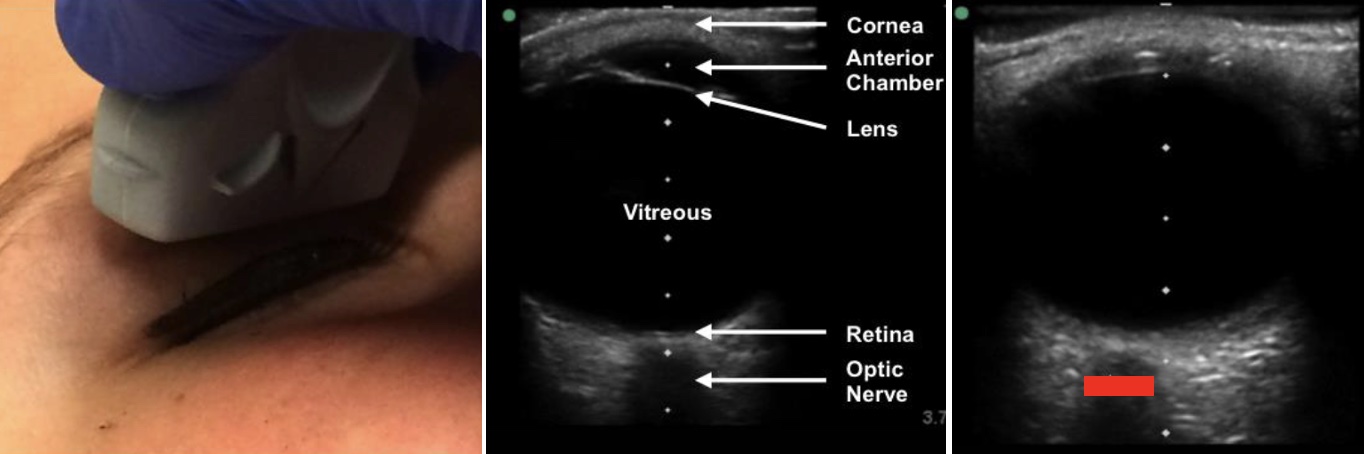
ONSD (Red Bar) 1
Management
Goal CPP > 60 mmHg (50-70 mmHg) to Avoid Secondary Brain Injury
- Goal ICP < 20 in General
Initial Measures
- IV Fluids (Normal Saline)
- Pressor Support and Avoid Hypotension
- Elevate Head-of-Bed to 30 Degrees – Support Adequate Venous Drainage
- Sedation and Analgesia – Decrease Metabolic Demand
- Maintain Normothermia – Fever Increases Metabolic Demand and Blood Flow
- Intermittent CSF Drainage (If an EVD is Present)
- Avoid:
- Steroids – Increase Mortality
- Lumbar Puncture – Can Precipitate Herniation
Secondary Options
- Osmotic Therapy
- Goal Na: 145-155
- Hypertonic Saline or Mannitol Boluses (Not Continuous)
- Avoid Mannitol (Diuretic) if Hypotensive or Hypovolemic
- Hyperventilate
- Goal PaCO2: 30-35
- Induces Cerebral Vasoconstriction
- Exchange Parenchymal Pressure Monitor (Bolt) for an External Ventricular Drain (EVD) to Allow Intermittent CSF Drainage
Refractory Treatment
- Neuromuscular Paralysis
- Barbiturate Coma
- Therapeutic Hypothermia
- Decompressive Craniectomy
- Improves Survival but More Survivors are Dependent on Others and Higher Risk of Unfavorable Outcomes (RESCUEicp and DECRA Trials)
References
- Bergmann KR, Milner DM, Voulgaropoulos C, Cutler GJ, Kharbanda AB. Optic Nerve Sheath Diameter Measurement During Diabetic Ketoacidosis: A Pilot Study. West J Emerg Med. 2016 Sep;17(5):531-41. (License CC BY-4.0)
