Fluid Responsiveness
Fluid Responsiveness
David Ray Velez, MD
Table of Contents
Definition and Assessment
Also Known as “Volume Responsiveness” or “Preload Responsiveness”
Definition
- The Ability of the Heart to Increase Cardiac Output or Stroke Volume in Response to Fluid Administration
- Exact Definitions Vary
- Goal of Fluid is to Improve Cardiac Output and Oxygen Delivery (DO2)
- If Not Responsive, Excessive Fluid Risks Fluid Overload with Pulmonary Edema and Associated Morbidity
- Can Be Difficult to Determine in Some Cases Such as Septic Shock with CHF
- Only About 50% of Unstable Critically Ill Patients Will Respond Positively to a Fluid Challenge
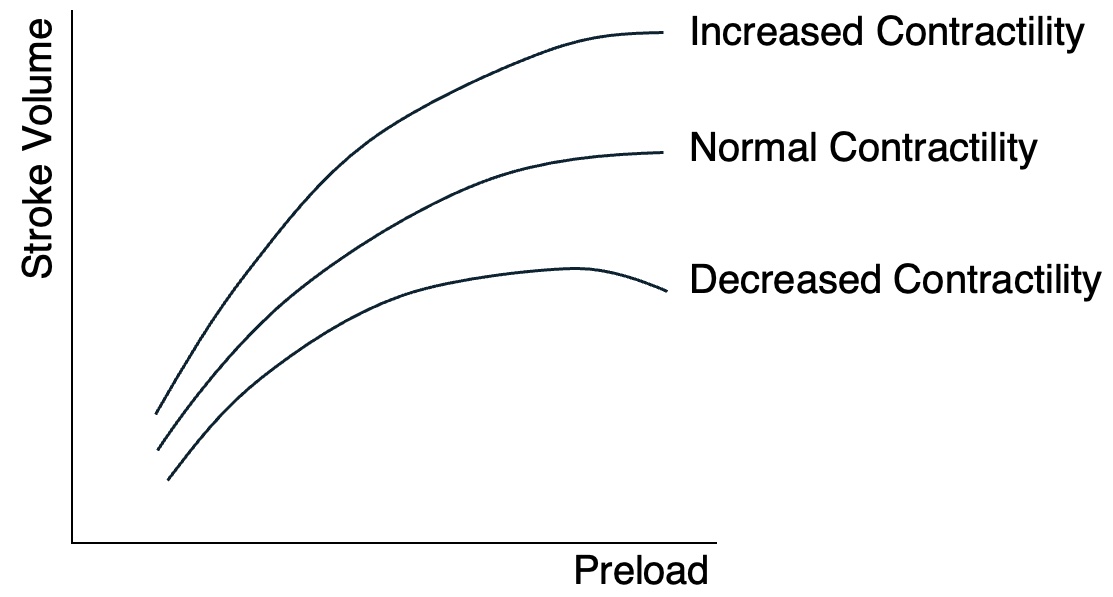
Frank-Starling Mechanism (Law)
- Describes How Stroke Volume and Cardiac Output Increases in Response to Increased End Diastolic Volume (Preload)
- The Basic Theory of Fluid Responsiveness
- The Vertical Segment is Preload Dependent and Will Respond to Fluid Administration
- The Horizontal Segment is Preload Independent and Will Not Respond to Fluid Administration
- Decreased Cardiac Contractility Decreases the Effect Additional Fluid Administration/Preload Will Have on Increasing the Stroke Volume and Excessive Preload Can Actually Cause a “Falling Off” with Decreased Stroke Volume
Fluid Challenge
- The Definitive Test of Fluid Responsiveness
- However, it Creates a Risk of Fluid Overload if Not Fluid Responsive
- Test: Patient Given a 500 cc Bolus of Fluid as Fast as Possible (Around 10-15 Minutes)
- Positive Results: 10% Increase in Cardiac Output or Stroke Volume
- Surrogate Measure (If No Pulmonary Artery Catheter or FloTrac): 10% Increase in Pulse Pressure on Arterial-Line
Static Assessment of Fluid Responsiveness
- *Static Assessments (Looking at a Static Moment in Time) are Generally Not Sensitive, Not Specific, and Have Limited Clinical Use in Determining Fluid Responsiveness
- Vital Signs (Heart Rate/Blood Pressure)
- Prior Urine Output
- Chest X-Ray/Lung Ultrasound – Looking for Pulmonary Edema to Determine Fluid Overload (Indicating Lack of Responsiveness)
- Late Marker of Fluid Overload
- Central Venous Pressure (CVP)
- Better Indicator of “Preload” and Not Necessarily “Preload Responsiveness”
- Extreme Values May Be More Reliable (< 6 Indicates Fluid Responsive and > 15 Indicates Not)
Dynamic Assessment of Fluid Responsiveness
- *Dynamic Assessments (Evaluating in Response to an Effect) are Generally More Clinically Reliable than Static Assessments Although Data to Support is Highly Variable
- Passive Leg Raise
- Volume/Pressure Variations:
- Stroke Volume Variation (SVV)
- Pulse Pressure Variation (PPV)
- Ventilator Simulations:
- End-Expiratory Occlusion test (EEOT)
- Tidal Volume Challenge (TVC)
- Point-of-Care Ultrasound (POCUS):
- IVC Collapsibility/Distensibility
- Internal Jugular Ultrasound
Frank-Starling Curve
Dynamic Assessment
Passive Leg Raise
- Technique:
- Patient Placed in a Semi-Recumbent Position with Head of Bed at 45 Degrees
- Head Lowered Supine/Flat and Legs Passively Raised to 45 Degrees
- Quickly Returns a Reservoir of Venous Blood into Central Circulation in 30-90 Seconds
- Positive Results: 10% Increase in Cardiac Output or Stroke Volume
- Surrogate Measure (If No Pulmonary Artery Catheter or FloTrac): 10% Increase in Pulse Pressure on Arterial-Line
- *The Most Well Validated Test of Fluid Responsiveness
Stroke Volume Variation (SVV)
- SVV (%) = (Maximum SV – Minimum SV) / Average SV
- Measured Using a Pulmonary Artery Catheter or FloTrac/Vigileo System
- Normal SVV: 10-13%
- < 10%: Unlikely to Be Volume Responsive
- > 13-15%: Likely to Be Volume Responsive
- Accurately Measured Only if on Controlled Mechanical Ventilation and in Normal Sinus Rhythm
- Use Contraindicated if Having Arrhythmias or Spontaneous Ventilation (Irregular Nature of Spontaneous Breaths Causes Variation)
Pulse Pressure Variation (PPV)
- PPV (%) = (Maximum PP – Minimum PP) / Average PP
- Pulse Pressure Can Be Used as a Surrogate for Stroke Volume if No Pulmonary Artery Catheter or FloTrac/Vigileo System are Being Used
- Generally Proportional but Relative Change in PP After Fluid Expansion May Not Accurately Approximate Change in SV Due to the Non-Linear Relationship of Left Ventricular Pressure to Volume
- Use is Otherwise Similar to SVV
- Normal PPV: 10-13%
- < 10%: Unlikely to Be Volume Responsive
- > 13-15%: Likely to Be Volume Responsive
- Accurately Measured Only if on Controlled Mechanical Ventilation and in Normal Sinus Rhythm
- Use Contraindicated if Having Arrhythmias or Spontaneous Ventilation (Irregular Nature of Spontaneous Breaths Causes Variation)
End-Expiratory Occlusion Test (EEOT)
- A 15-Second End-Expiratory Hold (Occlusion) is Performed on the Ventilator
- Simulates a Fluid Challenge by Preventing Inspiration and the Subsequent Preload Inhibition
- Increased Cardiac Output or Stroke Volume Predicts Volume Responsiveness
- Can Use Pulse Pressure on Arterial-Line as a Surrogate Measure (If No Pulmonary Artery Catheter or FloTrac)
- Must Be Able to Tolerate an End-Expiratory Hold
- Unreliable if Spontaneously Breathing, Prone, or Intra-Abdominal Hypertension
- Less Sensitive if Lung Compliance is Poor (ARDS, etc.)
Tidal Volume Challenge (TVC)
- Tidal Volume is Temporarily Increased to 8 mL/kg for 1 Minute
- Increased Intrathoracic and Transpulmonary Pressures:
- Decreased LV Afterload and a Transient Increase in LV Preload Due to Alveolar Blood Being Squeezed Out – Transient Increase in Stroke Volume (Highest in Inspiration)
- Decrease Venous Return/RV Preload and Increase RV Afterload – Causes a Decrease in Stroke Volume After a Few Heart Beats to Overcome Pulmonary Transit Time (lowest in Expiration)
- Increased Cardiac Output or Stroke Volume Predicts Volume Responsiveness
- Can Use Pulse Pressure on Arterial-Line as a Surrogate Measure (If No Pulmonary Artery Catheter or FloTrac)
- Can Also Assess Effect by SVV or PPV
- Risk for Lung Injury from Increased Volume and Pressure
- Unreliable if Spontaneously Breathing or Intra-Abdominal Hypertension
- Less Sensitive if Lung Compliance is Poor (ARDS, etc.)
Assessment by Point-of-Care Ultrasound (POCUS)
IVC Diameter
- A Static Measurement of IVC Diameter
- Normal Diameter: 13-17 mm and Not Completely Compressible
- < 13 mm: Likely to Be Volume Responsive
- > 25 mm: Unlikely to Be Volume Responsive
- Generally Poor Accuracy, Although Extreme Values (Flat vs Full) May Be More Predictive
IVC Collapsibility Index (Caval Index)
- Change in IVC Diameter Throughout the Respiratory Cycle in Spontaneously Breathing Patients
- IVC CI (%) = (Max – Min) / Max Diameter
- Maximum Diameter on Expiration
- Minimum Diameter on Inspiration
- Interpretation:
- Near 50-100% Indicatives Fluid Responsiveness
- Near 0% Indicatives Fluid Non-Responsiveness
- Positive Pressure Ventilation is a Contraindication – Positive Pressure on Inspiration Prevents IVC Collapse
IVC Distensibility Index
- Change in IVC Diameter Throughout the Respiratory Cycle in Mechanically Ventilated Patients
- IVC DI (%) = (Max – Min) / Min Diameter
- Maximum Diameter on Inspiration
- Minimum Diameter on Expiration
- Increase ≥ 18% Indicates Fluid Responsiveness
Other Ultrasound Evaluations
- Heart Ultrasound/Echocardiography
- End-Diastolic Volume (EDV) Assesses Preload
- Left Ventricular Outflow Tract (LVOT) Velocity Time Index (VTI) Estimates Stroke Volume
- Lung Ultrasound
- Evaluates for Pulmonary Edema to Determine Fluid Overload (Indicating Lack of Responsiveness)
- Carotid Artery Ultrasound
- Carotid Velocity Time Index (VTI) Can Estimate Stroke Volume – Easier to Perform than LVOT by Echo but Less Accurate
- Internal Jugular Vein Ultrasound
- Can Evaluate for IJ Diameter and Collapsibility During the Respiratory Cycle (Similar to IVC Evaluation)
- Generally Considered Less Reliable than IVC Evaluation
- Small IJ with Collapse Throughout the Respiratory Cycle is Likely to Be Volume Responsive
- Dilated IJ with No Collapse is Unlikely to Be Volume Responsive
- Can Evaluate for IJ Diameter and Collapsibility During the Respiratory Cycle (Similar to IVC Evaluation)
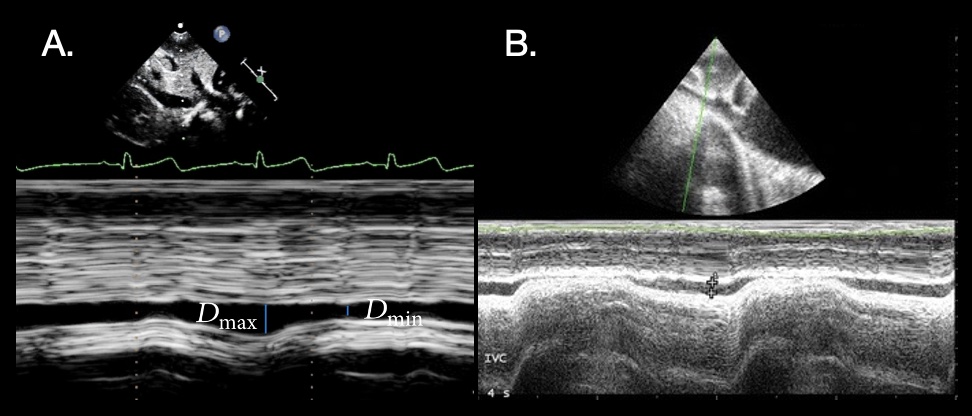
IVC Collapsibility POCUS: (A) Normal 1; (B) Collapse 2
References
- Gaspar HA, Morhy SS. The Role of Focused Echocardiography in Pediatric Intensive Care: A Critical Appraisal. Biomed Res Int. 2015;2015:596451. (License: CC BY-3.0)
- Mok KL. Make it SIMPLE: enhanced shock management by focused cardiac ultrasound. J Intensive Care. 2016 Aug 15;4:51. (License: CC BY-4.0)
