Esophagus Trauma
Esophagus Trauma
David Ray Velez, MD
Table of Contents
Background
The Majority are Due to Penetrating Trauma
Site
- Cervical Esophagus – Most Common
- Thoracic Esophagus – Less Common Due to Bony Protection
- Abdominal Esophagus – Least Common
Nearly All (98%) Have Other Associated Injuries
AAST Esophagus Injury Scale
- *See AAST
- Injury Scale is Under Copyright
Diagnosis
Signs/Symptoms
- Pain in the Neck, Chest, or Abdomen
- Dysphagia – Pain with Swallowing
- Nausea and Vomiting
- Hematemesis
- Dyspnea
- Cough
- Subcutaneous Emphysema
- Presentation is Generally Nonspecific
Delay in Diagnosis is Common and Requires a High Index of Suspicion
Diagnosis
- Start with a Water-Soluble Contrast Esophagram
- Can Pull NG Back to the Proximal Esophagus Before Contrast Instillation if Intubated
- If Negative but High-Suspicion of Injury: Repeat Esophagram with Dilute-Barium
- If Negative Again: Esophagoscopy
Specificity/Sensitivity
- Contrast Studies Alone Have High False-Negative Rates (25%)
- Esophagoscopy Has a High Negative Predictive Value (100%) but Low Positive Predictive Value (33%)
- A Negative Esophagram AND Esophagoscopy Have a Near 100% Specificity
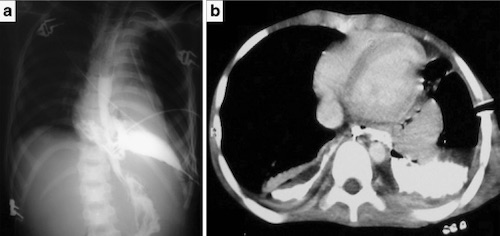
Traumatic Esophagus Perforation with Oral Contrast Extravasation 1
Treatment
The Primary Treatment is Surgical Repair Reinforced with Buttress and Drainage
Surgical Approach to the Esophagus
- Cervical Esophagus: Left Cervical Incision Along the Anterior Border of the Sternocleidomastoid (SCM) Muscle
- Thoracic Esophagus (Upper 2/3): Right Posterolateral Thoracotomy – Avoids the Aorta on the Left
- Thoracic Esophagus (Lower 1/3): Left Posterolateral Thoracotomy – The Aorta Transitions to the Right Distally
- May Be Able to Repair Through a Laparotomy Alone for Distal Injuries at the Esophagogastric Junction
Surgical Repair
- The First Step is to Extend the Myotomy to See the Full Length of Mucosal Injury
- The Muscular Defect is Almost Always Smaller than the Mucosal Defect
- Close the Defect in Two Layers without Tension
- Inner Absorbable Suture and Outer Permanent Suture
- The Submucosa is the Strength Layer – There is No Serosa in the Esophagus
- Transverse Repair is Preferred for Small Defects, but Large Injuries May Require Longitudinal Repair
- The Blood Supply is Longitudinal Through the Submucosa – Allows Full Mobilization
- Explore Circumferentially in Penetrating Injury to Verify No Back-Wall Injury
Buttress
- Esophageal Repairs Should Be Buttressed to Strengthen and Enhance Healing Given No Serosal Layer Which Increases the Risk of Postoperative Leak
- Neck: Strap Muscles or Sternocleidomastoid (SCM) Muscle
- Proximal Thorax: Intercostals or Rhomboid Muscle
- Muscle Flaps are Preferred – Less Friable and Provide More Bulky Coverage
- Other Less Desirable Options: Pericardium or Pleura
- Distal Thorax or Abdomen: Stomach (Nissen Fundoplication) or Diaphragm
Drainage
- Neck: Penrose or JP Drain
- Thoracic: Chest Tubes
- Abdomen: JP Drain
Damage Control Options
- Neck: Cervical Esophagostomy (Spit Fistula)
- Loop Esophagostomy If Able – Allows Easier One-Stage Closure as an End Esophagostomy Requires Complex Closure
- Thoracic: Large T-Tube (Creates a Controlled Fistula)
The Use of Endoluminal Esophageal Stents is Evolving but May Be an Appropriate Alternative for Damage Control
References
- Oikonomou A, Prassopoulos P. CT imaging of blunt chest trauma. Insights Imaging. 2011 Jun;2(3):281-295. (License: CC BY-4.0)
