Deep Vein Thrombosis (DVT)
Deep Vein Thrombosis (DVT)
David Ray Velez, MD
Table of Contents
Definition
Definitions
- Venous Thromboembolism (VTE): Blood Clot within the Venous System
- Deep Vein Thrombosis (DVT): Blood Clot within the Deep Venous System
- Pulmonary Embolism (PE): Blood Clot Occlusion of the Pulmonary Arteries, Most Often Due to a DVT
Provoked Definition
- Provoked: Caused by a Known Event (Surgery, Trauma, etc.)
- Unprovoked: No Known Provoking Event
Location Definition
- Proximal DVT:
- Leg: Iliac, Femoral, or Popliteal Veins
- Arm: Axillary or Subclavian Veins
- Distal DVT:
- Leg: Deep Veins Below the Knee
- Arm: Brachial or More Distal Veins
- *Basilic, Cephalic, and Saphenous Veins are Superficial Veins (Not Considered a DVT)
Risk Factors
Virchow’s Triad
- Describes the Three Primary Factors that Lead to Increased Risk of Venous Thromboembolism (VTE)
- Triad:
- Hypercoagulability
- Venous Stasis – Reduced Flow Decreases the Interaction of Cell Proteins and Natural Anticoagulant Pathways on Endothelial Cell Surfaces
- Endothelial Wall Injury – Alters Blood Flow Dynamics and Creates Turbulence
Acquired Hypercoagulability
- Smoking – The Most Common Cause of Acquired Hypercoagulability
- Inflammation/Infection
- COVID-19
- Prolonged Immobilization
- Prolonged Sitting
- Extended Travel
- Bedridden Medical Conditions
- Hospitalization
- Advanced Age
- Recent Major Surgery – Due to a Transient Release of Tissue Factor
- Trauma – Even Minor Injuries Can Increase Risk
- Spinal Cord Injury – The Highest Risk Injury in Trauma
- Malignancy – From Production of Procoagulant Substances
- Pregnancy
- Inflammatory Bowel Disease (IBD)
- Antiphospholipid Syndrome
- Heart Failure
- Severe Liver Disease
- Obesity
- Chronic Kidney Disease and Nephrotic Syndrome
- IV Drug Abuse
- Drugs:
- Oral Contraceptives
- Hormone Replacement Therapy
- Testosterone
- Tamoxifen
- Steroids
- Antidepressants
Inherited Thrombophilia
- Factor V Leiden – The Most Common Inherited Thrombophilia
- Prothrombin G20210A
- Antithrombin-III Deficiency
- Protein C Deficiency
- Protein S Deficiency
Additional Risk Factors
- Central Venous Catheter (CVC)
- Post-Thrombotic Syndrome: DVT Induced Injury to Valves Producing Chronic Venous Insufficiency
- May-Thurner Syndrome: Left Iliac Vein Thrombosis Due to Compression by Right Iliac Artery
Presentation
Location
- Most Common Site: Calf
- Left Side is 2x More Common Than Right
Symptoms
- Swelling
- Pain
- Warmth
- Erythema
Homans Sign
- Pain with Foot Dorsiflexion
- No Diagnostic Value – Poor Sensitivity and Specificity
Phlegmasia
- Phlegmasia Alba Dolens
- White Discoloration, Painful, and Swollen
- Indicates Early DVT Impairment of Arterial Supply
- Phlegmasia Cerulea Dolens
- Blue Discoloration, Painful, and Swollen
- Indicates Late DVT Impairment of Arterial Supply and Impending Gangrene
- Half Have Malignancy
- Mnemonic: USA! (Red, White, and Blue)
- Represents DVT Color Changes by Timing and Severity
- Red – Swollen Red DVT
- White – Phlegmasia Alba Dolens
- Blue – Phlegmasia Cerulea Dolens
- Cerulea is “Cruel” and the Worst

DVT: (A) Phlegmasia Alba Dolens 1; (B) Phlegmasia Cerulea Dolens 2
Diagnosis
Diagnosis: Ultrasound (US)
- Labs and D-Dimer are Not Specific and Generally Not Useful in the Surgical Setting
Ultrasound (US) Findings
- Intramural Thrombus
- Noncompressible Veins
- Venous Dilation
- No Flow
Chronicity by Ultrasound (US)
| Acute | Chronic | |
| Echolucency | Hypoechoic | Bright |
| Heterogeneity | Homogenous | Heterogenous |
| Attachment | Poor | Firm |
| Borders | Smooth | Irregular |
| Rigidity | Nonrigid | Rigid |
| Veins | Dilation | Small/Contracted |
| Collaterals | Small | Large |
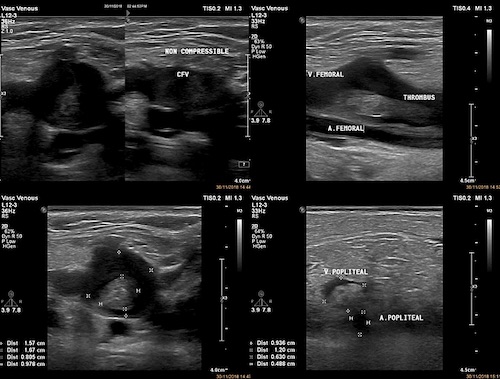
Femoral DVT on US 1
Treatment
Prophylaxis
Treatment
- Primary Treatment: Anticoagulation
- Distal DVT’s Do Not Require Anticoagulation Unless They are Symptomatic
- Consider Serial US Every 2 Weeks to Monitor Progression
- Phlegmasia Cerulea Dolens: Catheter-Directed Thrombolytics
- Surgical Thrombectomy May Be Required for an Immediately Threatened Extremity
Duration of Anticoagulation
- Provoked First Episode: Short-Term (3-6 Months)
- Unprovoked or Second Episode: Long-Term (12 Months)
- Hypercoagulable Disorder or Third Episode: Life Long
Choice of Agent
- General Options:
- Unfractionated Heparin
- Low Molecular Weight Heparin (Lovenox)
- Fondaparinux
- Rivaroxaban
- Apixaban
- Warfarin/Coumadin – Cannot Be the Sole Initial Treatment
- Malignancy: Low Molecular Weight Heparin (Lovenox)
- Pregnancy: Heparin or Low Molecular Weight Heparin (Lovenox)
- Warfarin is Teratogenic
*May-Thurner Syndrome Managed with Venography, Thrombolysis/Thrombectomy & Left Iliac Stent
IVC Filter
Goal: PE Prophylaxis
Indications
- Acute DVT with Absolute Contraindication to Anticoagulation
- Active Bleeding
- Acute Intracranial Hemorrhage
- Major Trauma
- High Bleeding-Risk Surgery
- Recurrent VTE Despite Therapeutic Anticoagulation
Placement
- Access Through Right IJ – Most Direct Access
- Infrarenal IVC Position
- Generally Preferred for Most Cases
- Minimize Risk of Filter Obstruction Occluding the Renal Veins
- Suprarenal IVC Position
- Used for a Renal Vein Thrombosis
- Used in Pregnancy – To Avoid Contact with a Gravid Uterus
Removal
- Filters Should Be Removed as Soon as Protection is No Longer Needed
- Low Overall Retrieval Rate: 25-34%
- Best Predictor of Removal: Thrombosis Clinic Follow Up Appointment
- Highest Risk of Difficult Removal: Placement > 7 Months
Complications
- Increases DVT Risk
- IVC Thrombosis
- Filter Migration
- Filter Erosion
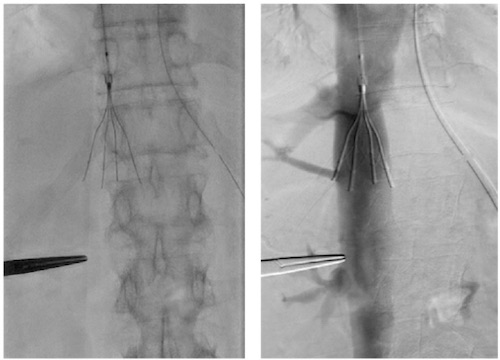
IVC Filter Placement 3
References
- Suciadi L P, Aristo A N (March 24, 2021) Phlegmasia Alba Dolens Complicating Rhabdomyolysis. Cureus 13(3): e14080. (License: CC BY-4.0)
- Yang SS, Yun WS. Surgical Thrombectomy for Phlegmasia Cerulea Dolens. Vasc Specialist Int. 2016 Dec;32(4):201-204. (License: CC BY-NC-4.0)
- Kishima H, Fukunaga M, Nishian K, Saita T, Horimatsu T, Sugahara M, Mine T, Masuyama T. Aspiration thrombectomy in a patient with suprarenal inferior vena cava thrombosis. Case Rep Cardiol. 2015;2015:495065. (License: CC BY-3.0)
