Central Line (Central Venous Catheter/CVC)
Central Line (Central Venous Catheter/CVC)
David Ray Velez, MD
Table of Contents
Definitions and Function
Anatomy
- Internal Jugular (IJ) Vein
- Lies Under the Sternocleidomastoid Muscle (SCM)
- Vein Runs Anterior and Lateral to the Carotid Artery
- Subclavian (SC) Vein
- Runs Under Clavicle
- Subclavian Artery and Brachial Plexus Are Deep to the Vein
- Femoral Vein
- Runs Medial to the Femoral Artery
- From Lateral-to-Medial: Nerve, Artery, Vein, Empty Space, Lymphatics
Types of Central Lines
- Non-Tunneled CVC
- A Catheter Placed Directly from the Skin into the Vein
- Placed at Bedside
- Higher Risk of Infection and Generally Considered a Temporary Measure for 2-3 Weeks
- *Generally What is Meant When Referring to a “Central Line”
- Tunneled CVC
- A Catheter is Tunneled Under the Skin for a Distance Before Entering the Vein at a Separate Site
- Placed by IR or in the OR
- Lower Risk of Infection and May Be Used for a Longer-Term
- Peripherally Inserted Central Catheter (PICC)
- Longer Line Placed Peripherally into an Arm Vein
- Less Invasive and Lower Infection Risk
- Smaller Caliber Lumens
- Often Used if Anticipating Long-Term Need (TPN or Antibiotics)
- Subcutaneous Port (Port-a-Cath)
- Completely Tunneled Catheter with Port Beneath the Skin and No Exposed Ports
- Placed Under Anesthesia
- Lower Infection Risk than Tunneled or Non-Tunneled CVC
- Longer Patency – Ideal for Chemotherapy
Flow Rate
- Hagen-Poiseuille Equation
- Flow (Q) = ΔP x πr4 / 8 µL
- P = Pressure, r = Radius, µ = Viscosity, L = Length
- Directly Related to Radius4
- Inversely Related to Length1
- Flow (Q) = ΔP x πr4 / 8 µL
- Increased Flow with Higher Radius (Strongest Factor) and Lower Length
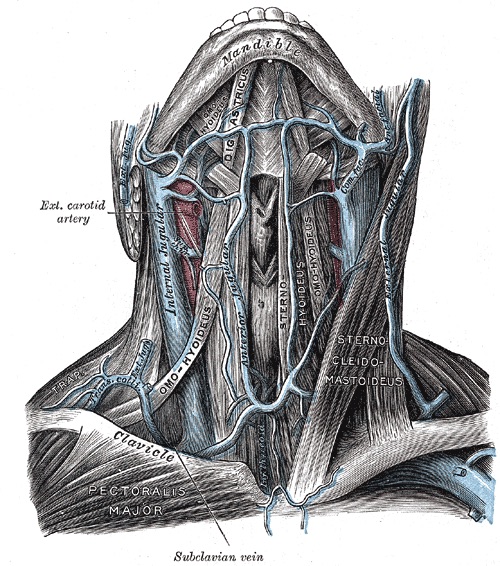
Internal Jugular Vein and Subclavian Vein
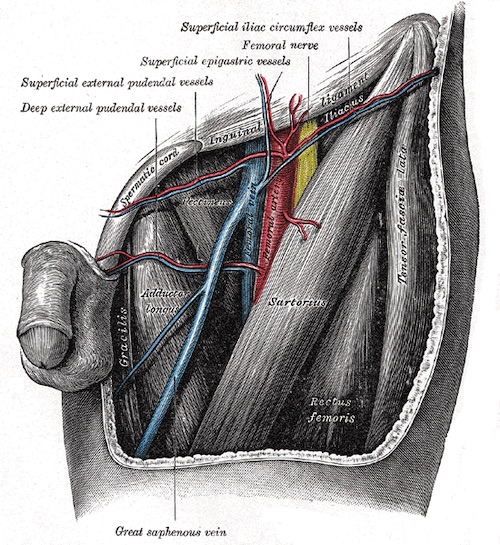
Femoral Vein
Choice of Line and Site
Choice of Line
- General Use in the ICU: 7 Fr Triple-Lumen is Standard
- Multiple Lumens Allow for Infusion of Multiple Agents at the Same Time
- Hemorrhagic Shock: Large-Bore (8-11 Fr) Single-Lumen Catheter
- Often Referred to as a “Cordis” (The Manufacturing Company)
- Used in Trauma, GI Bleed, Ruptured AAA, etc.
- Largest Bore Allows the Most Rapid Blood Transfusion
- Hemodialysis Access: Medium-Large Bore (14.5 Fr) Double-Lumen Catheter
- Two Lumens are Large Enough to Support Dialysis Flow Rates
- May Have an Additional Smaller Lumen Port for Additional Access
- “VasCath”: Placed in a Typical Non-Tunneled-Fashion for Short-Term Access
- Generally What is Initially Placed While in the Hospital
- “PermaCath”: Placed in a Tunneled-Fashion for Longer Access
- Generally Placed When Anticipating Discharge and Long-Term Need
- Two Lumens are Large Enough to Support Dialysis Flow Rates
- Long-Term Need for TPN or Antibiotics: PICC Generally Preferred Over a Traditional CVC
Choice of Site
- Internal Jugular (IJ) Vein
- Most Often the Preferred Site Under Ultrasound Guidance if Able
- Straight Path into the SVC Allows a Low Rate of Catheter Malposition
- Able to Provide Compression for Bleeding Easier than the Subclavian
- Subclavian (SC) Vein
- Lowest Infection Risk
- Lowest DVT Risk
- Highest Risk of Mechanical Complication (Pneumothorax, etc.)
- *If Patient Already Has a Pneumothorax and Chest Tube – Strongly Consider Placing Central Line on the Ipsilateral Side (If Placement is Complicated by Pneumothorax it is Already Treated – “Free Shot”)
- Femoral Vein
- Lowest Mechanical Complication Risk
- IJ and Femoral Have a Similar Risk of Infection (Debated)
Placement/Technique
Techniques
- Blind Placement: Based Solely on Anatomy and Palpation without US Guidance
- Ultrasound Guidance: Placed Using an Ultrasound in Real-Time
- Benefits to Ultrasound Use:
- Decreased Complication Rate
- Decreased Failure Rate
- Increased First-Pass Success
- Should Always be Utilized if Available
- Benefits to Ultrasound Use:
- *Either Method Utilizes a Seldinger Technique
Position/Prep
- Supine or Head-Down 10-20 Degrees
- For Subclavian Vein CVC, Arm Should be Completely Adducted
- Having an Assistant Pull the Ipsilateral Arm Inferiorly During Placement Can Provide Help
- Procedure Should be Performed in a Sterile Manner Unless Absolutely Unable (“Dirty Lines” Used in Trauma for a Crashing Patient in Hemorrhagic Shock)
Blind Placement
- Internal Jugular (IJ) Vein
- Insertion:
- Anterior Approach: Along the Medial Border of the SCM, 2-3 Fingerbreadths Above the Clavicle
- Central Approach: The Apex of the Bifurcation of the SCM Heads
- Angle: 30-45 Degrees
- Aim: Ipsilateral Nipple
- *Palpate the Carotid Artery During Placement (Vein Should be Lateral to the Pulse)
- Insertion:
- Subclavian Vein
- Insertion: 2-3 cm Below Midpoint of Clavicle (1-2 cm Lateral of Bend About the Deltopectoral Fascia)
- Aim: Just Deep to Sternal Notch
- If Clavicle is Hit, Withdraw and March Down
- Femoral Vein
- Insertion: 1-2 cm Below the Inguinal Ligament and 1 cm Medial to the Femoral Artery Pulse (About 2 Finger-Breadths Lateral to the Pubic Tubercle
- Angle: 30-45 Degrees
- *Palpate the Femoral Artery During Placement (Vein Should be Medial to the Pulse)
Seldinger Technique
- Needle
- Puncture Vein with a Hollow Introducer Needle
- Attach Syringe with Gentle Negative Pressure During Advancement
- Dark Non-Pulsatile Blood Indicates Venipuncture (Caution: Arterial Blood in Hypoxic Patients May Also be Dark)
- Guidewire
- Pass a Guidewire Through the Needle
- Withdraw the Needle Over the Guidewire, Leaving the Guidewire in Place
- Always Maintain Control of the Guidewire During Placement – Should Never Completely Enter the Vein
- Dilate the Tract
- Make a Small Skin Incision at the Entry Site
- Pass a Dilator Over the Guidewire and Remove it to Dilate the Tract
- Place the Catheter
- Pass Catheter Over the Guidewire
- Withdraw Guidewire
- Cap the Ports
- Confirm the Each Port is Able to Withdraw Blood and Flush
- Suture Catheter to Skin and Place a Sterile Dressing
- *Always Obtain Post-Procedure Chest XR to Confirm Appropriate Positioning and Look for Pneumothorax (Not Necessary for Femoral Access)
Goal CVC Tip Location
- Internal Jugular/Subclavian: 1-2 cm Above the Right Atrium-SVC Junction
- Seen as Just Above the Carina on Chest XR
- Femoral: Generally Not Evaluated
Approximate Insertion Length
- Equation Based on Height (cm):
- Right SC: Height/10 – 2 cm
- Right IJ: Height/10
- Left SC: Height/10 + 2 cm
- Left IJ: Height/10 + 4 cm
- General Lengths:
- Right SC: 11-14 cm
- Right IJ: 13-15 cm
- Left SC: 15-17 cm
- Left IJ: 17-18 cm
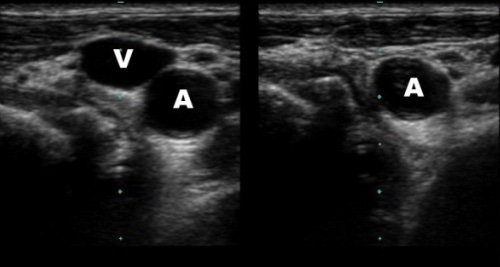
US Guidance Showing Compressible IJ (V) and Noncompressible Carotid (A) 1
Complications
Carotid Cannulation (Arterial Injury)
- Can Cause Life-Threatening Hemorrhage
- Reduce Risk by Using Ultrasound-Guidance for Placement
- Diagnosis:
- ABG from the Catheter Showing Arterial Rather than Venous Values
- Pressure Transducer Attached to the Catheter Showing an Arterial Waveform
- Chest XR Showing Catheter to the Left of the Spine
- Treatment:
- Cannulation with Needle or Guidewire Only: Remove and Hold Pressure for 5-10 Minutes
- Cannulation with Dilator or Catheter: Remove Under Fluoroscopy or in OR

CVC in the Aorta
Malposition
- Tip Abutting into the Wall of the Superior Vena Cava
- Risk for SVC Puncture
- Treatment: Retract to the Innominate Vein (Do Not Advance – Risk for Introducing Bacteria and Infection)
- Tip in the Right Atrium
- Risk for Atrial Wall Puncture
- Treatment: Retract to the Right-Atrium-SVC Junction
Pneumothorax (PTX)
- Risk: 1-6.6% (Higher Risk in Emergency Setting or if Multiple Needle Passes are Required to Find the Vein)
- Treatment:
- Asymptomatic and Small (< 3 cm): Repeat Chest XR in 6 Hours to Monitor Progression
- Supplemental Oxygen May Enhance Reabsorption – Reduces Partial Pressure of Nitrogen for a Diffusion Gradient
- Symptomatic or Large (> 3 cm): Chest Tube
- Smaller Tubes (8-14 Fr) are Generally Preferred for PTX
- Asymptomatic and Small (< 3 cm): Repeat Chest XR in 6 Hours to Monitor Progression
- *See Pneumothorax (PTX)
Cardiac Tamponade
- From Puncture of the Right Atrium
- *See Cardiac Tamponade
Catheter-Related Thrombosis (CRT)
- Risk Factors:
- Hypercoagulable State (Malignancy, Sepsis, etc.)
- Increased Lumen Diameter
- Left Sided Placement
- Malposition with Tip Above the Junction of the SVC and Atrium
- Multiple Insertion Attempts
- Presentation:
- Asymptomatic – Most Common
- Swelling of the Head, Neck, or Limb
- Headache
- Localized Pain or Numbness
- Superficial Venous Distention
- Limb Erythema
- Catheter Malfunction – Difficulty with Infusion or Aspiration
- Complications:
- Pulmonary Embolism (PE) (10-15%)
- Infection
- Post-Thrombotic Syndrome
- Loss of Access
- Diagnosis: Duplex Ultrasound
- Contrast Venogram is the Gold Standard Test – Used if Duplex is Negative Despite High Suspicion
- Treatment: Systemic Anticoagulation and Remove Catheter (If Able)
- May Consider Keeping Catheter Only if it is Functional, Well Positioned, and Not Infected
- Line Must Be Removed if Anticoagulation is Contraindicated, the Thrombosis is Limb/Life Threatening, or Symptoms Do Not Resolve
Air Embolism
- Presentation: Hypoxemia and Respiratory Distress
- “Millwheel” Murmur: Loud Churning – Late Finding
- Neurologic Abnormalities if Embolized to Arterial System
- Diagnosis: Demonstration of Intravascular Air with a Known Risk Factor
- Often Rapidly Absorbed Prior to Imaging
- TEE is the Most Sensitive Test
- End Tidal Nitrogen Rises (If Available) Before End Tidal CO2 Decreases
- Treatment: Reposition and Supportive Care (Supplemental Oxygen)
- Repositioning:
- “Durant’s Maneuver” – Left Lateral Decubitus
- Steep Trendelenburg – Head Down
- Goal: Trap Air in the Right Ventricle
- If Hemodynamically Unstable Can Attempt Aspiration Through a Central Venous Catheter
- *See Air Embolism
Central Line-Associated Bloodstream Infection (CLABSI)
- Also Known as Catheter-Related Bloodstream Infection (CRBSI)
- Risk Increases with Duration of Placement (However there is No Indication for Routine Catheter Changing Based on the Number of Days)
- Skin Colonization is the Most Common Source
- Most Common Organisms:
- Coagulase-Negative Staphylococci (CoNS/S. epidermidis) (Most Common)
- Staphylococcus aureus
- Enterococci
- Candida
- Klebsiella
- Escherichia coli
- Enterobacter
- Pseudomonas
- Risk Factors:
- Duration of Catheterization
- Non-Sterile Insertion
- Poor Catheter Cares
- Immune Compromised/Neutropenic
- Malnutrition
- Femoral or IJ Location (Lowest for Subclavian)
- Presentation:
- Inflammation and Purulence at the Catheter Insertion Site
- Fever
- Sepsis (Often Sudden Onset)
- Complications:
- Septic Thrombophlebitis
- Infective Endocarditis
- Diagnosis: Obtain Two Peripheral Blood Cultures from Separate Sites Before Antibiotic Initiation
- Increased Risk of Contamination if Drawing from the Central Line
- Catheter Tip Cultures are Not Recommended – Low Positive Predictive Value
- A Single Coagulase-Negative Staphylococci (CoNS) Culture is Often a Contaminant and Should Consider Repeating the Cultures
- Consider Infective Endocarditis if Bacteremia is Persistent > 48-72 Hours
- Prevention:
- Remove as Soon as Possible
- Use Sterile Technique in Placement
- Use Ultrasound Guidance
- Chlorhexidine-Impregnated Dressings
- Use of Antimicrobial-Impregnated Central Lines
- Disinfect Hubs and Ports Before Accessing
- Use an Antiseptic-Containing Hub or Port to Cover Connectors
- Interventions Without Proven Benefit:
- Prophylactic Antibiotics
- Routine Replacement of Central Lines
- Daily Bathing with Chlorhexidine
- Securing the Catheter with a Suture – Creates Another Wound
- Treatment: Catheter Removal and Antibiotics
- *For CoNS – May Consider Withholding Antibiotics and Just Removing the Central Line – No Increased Risk of Complications or Recurrence
- If Clinically Unable to Remove the Catheter – Consider Exchange Over a Guidewire
- *See Central Line-Associated Bloodstream Infection (CLABSI)
References
- Gillman LM, Blaivas M, Lord J, Al-Kadi A, Kirkpatrick AW. Ultrasound confirmation of guidewire position may eliminate accidental arterial dilatation during central venous cannulation. Scand J Trauma Resusc Emerg Med. 2010 Jul 13;18:39. (License: CC BY-2.0)