Cardiac Tamponade
Cardiac Tamponade
David Ray Velez, MD
Table of Contents
Pathophysiology
Definition: Pericardial Fluid Accumulation Causes Increased Pressure and Impairs Cardiac Filling with Reduced Stroke Volume
Pathophysiology
- Cardiac Filling Impeded by Pericardial Fluid Causing Compression of the Cardiac Chambers
- Impairs Filling Once the Pericardial Pressure Exceeds the Diastolic (Filling) Pressure
- First Sign of Tamponade: Decreased Right Atrium Filling (Lowest Pressure of the Four Chambers and the First to Collapse)
- Speed of Accumulation:
- Rapid Accumulation of Even a Small Amount of Blood is Higher Risk for Collapse
- Even Larger Volumes Can Be Well Tolerated if They Accumulate Slowly Over Weeks-Years
- May Serve a Protective Effect in Penetrating Cardiac Injury to Limit Extra-Pericardial Hemorrhage
Phases
- Phase I: Increased Pericardial Pressure
- Output Maintained by Tachycardia, Increased SVR, and Filling Pressure
- Phase II: Diminished Cardiac Output
- Phase III: Intrapericardial Pressure Approaches Ventricular Filling Pressure
- Causes Cardiac Arrest from Profound Coronary Hypoperfusion
Causes
- Pericardial Effusion
- Trauma
- Post-Cardiac Surgery
- Myocardial Infarction (MI)
- Dissecting Aortic Aneurysm
- Pericarditis (Bacterial or Viral)
- Malignancy
- Autoimmune Disease
- Idiopathic
Diagnosis
Symptoms
- Chest Pain
- Dyspnea
- Fatigue
- Syncope
Physical Exam
- The Majority of Patients are Tachycardic
- Hypotension is Variable and is Often Not Present if Tachycardia is Able to Compensate for the Decreased Stroke Volume
- Physical Exam Findings in General are Neither Highly Sensitive nor Specific
- Pulsus Paradoxus: Decreased BP > 10 mmHg During Inspiration (Normal < 10 mmHg)
- Inspiration Increases Venous Return and Enlarged RV Impairs LV Filling
- Beck’s Triad:
- Jugular Venous Distention (JVD)
- Muffled Heart Sounds
- Hypotension with Narrow Pulse Pressure
- Kussmaul’s Sign: JVD Upon Inspiration
Diagnosis
- Primary Testing:
- Ultrasound (Echocardiography, POCUS, FAST) – The Primary Tool for Diagnostic Evaluation
- Chest Xray
- EKG
- Highly Suggestive if There are Clinical Signs/Symptoms of Tamponade with Ultrasound Showing Pericardial Effusion and Echocardiographic Signs of Tamponade
- Diagnosis is Only Definitively Confirmed by Clinical Response to Pericardial Fluid Drainage
Subxiphoid Pericardial Window
- *See Subxiphoid Pericardial Window
- Used in Trauma as a Diagnostic Tool, Not Therapeutic
- Less Commonly Preformed Now; But Consider if FAST is Equivocal
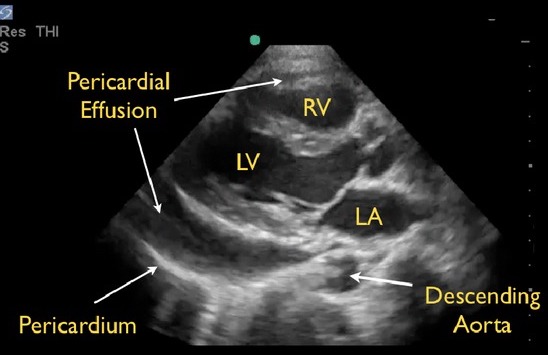
Pericardial Effusion on POCUS 2
Treatment
Traumatic Cardiac Tamponade
- Median Sternotomy
- The Primary Treatment for Cardiac Tamponade in Trauma
- Avoid Intubation Until in the OR and Already Prepped – Can Rapidly Decompensate Upon Induction
- Pericardiocentesis
- Generally Not Used in Trauma
- May Consider Pericardiocentesis to Temporize Prior to the OR if Acutely Unstable
- *See Pericardiocentesis
- Resuscitative Thoracotomy
- May Require Resuscitative Thoracotomy for Sudden Decompensation or Cardiac Arrest Prior to the OR
- *See Resuscitative Thoracotomy
Non-Traumatic Cardiac Tamponade
- Pericardiocentesis
- The Primary Treatment for Cardiac Tamponade Outside of Trauma
- *See Pericardiocentesis
- Fluid Bolus May Be Able to Temporarily Support While Awaiting Definitive Management
- Indications for Surgical Median Sternotomy:
- Concerned for Bleeding/Traumatic Injury
- Inaccessible to Pericardiocentesis
- Effusion Small or Loculated
- Need for Biopsy
- Coagulopathic
References
- COVER: BruceBlaus. Wikimedia Commons. (License: CC BY-3.0)
- Seif D, Perera P, Mailhot T, Riley D, Mandavia D. Bedside ultrasound in resuscitation and the rapid ultrasound in shock protocol. Crit Care Res Pract. 2012;2012:503254. (License: CC BY-3.0)