Cardiac Arrest
Cardiac Arrest
David Ray Velez, MD
Table of Contents
Classification
Shockable Rhythms
- Pulseless Ventricular Tachycardia (pVT)
- Ventricular Fibrillation (VF/V-Fib)
Non-Shockable Rhythms
- Asystole
- Pulseless Electrical Activity (PEA)
EKG Patterns
Pulseless Ventricular Tachycardia (pVT)
- Heart Rate > 100 bpm
- Wide QRS Complex (≥ 120 ms)
- No Fixed Relationship of P Wave and QRS Complex
- *No Palpable Pulse

Ventricular Tachycardia (VT/V-Tach)
Ventricular Fibrillation (VF/V-Fib)
- Sudden Chaotic Irregular Deflections
- No Identifiable P Waves, QRS Complexes or T Waves
- Rate 150-500 bpm
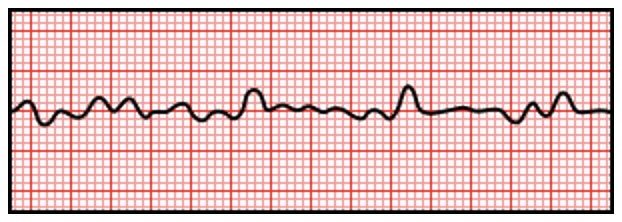
Ventricular Fibrillation
Asystole
- No Waveform
- Only an Isoelectric “Flat Line”
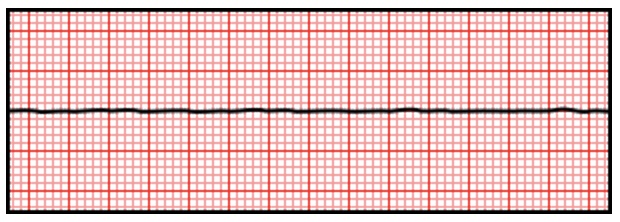
Asystole
Pulseless Electrical Activity (PEA)
- Sufficient Electrical Discharge to Maintain a Notable Rhythm
- *No Palpable Pulse
Prognosis
True Prognosis
- Survival to Discharge:
- Out-of-Hospital Cardiac Arrest: 10-12%
- In-Hospital Cardiac Arrest: 20-25%
- Majority of Survivors Have Some Degree of Brain Injury and Impaired Consciousness
- Shockable Rhythms (pVT and VF) Have a Higher Chance of Survival than Asystole/PEA
- Factors with High Specificity for Poor Neurologic Outcomes After ROSC:
- Absent or Extensor Motor Response After 72 Hours
- Absent Pupillary or Corneal Reflexes After 72 Hours
“As Seen on TV”
- The Public Often Has Falsely High Expectations
- In the Media:
- 46-75% Regain Spontaneous Circulation
- 67% Appear to Survive to Discharge
- Minimal Depiction of the Poor Medium-Long Term Outcomes
- Patient and Family Members Often Require Significant Education on Cardiac Arrest and Code Status
Treatment
General Treatment
- Follow ACLS Guidelines
- Start Chest Compressions Immediately
- Give Supplemental Oxygen (Bag Mask Ventilation)
- Treat Any Reversible Causes
- Pulse/Rhythm Check Every 2 Minutes
Appropriate Compressions
- At Least 2 Inches Depth
- At Least 100 per Minute
- *Can Compress to the Rhythm of the 1977 Song “Stayin’ Alive” by the Bee Gees to Maintain the Appropriate Rate – The Song Has About 103 Beats per Minute
- Maintain a Minimum Chest Compression Fraction of 60% (Time Spent Delivering Compressions During CPR)
Pulse/Rhythm Check
- Pauses Should Not Exceed 10 Seconds
- Continue Chest Compressions Immediately After Any Shock
- Rhythms:
- Shockable Rhythms: pVT and VF
- Non-Shockable Rhythms: Asystole and PEA
- Defibrillation Dose:
- Initial Dose: Biphasic 120-200 J
- Higher Subsequent Doses May Be Considered
Medication Therapy
- Epinephrine
- The Primary Agent Given for All Causes of Cardiac Arrest
- Dose: 1 mg IV/IO
- Give Initially and Repeat Every 3-5 Minutes
- Amiodarone
- Given Only for Shockable Rhythms (pVT/VF) and Not for Asystole or PEA
- Dose: 300 mg (First Dose) and 150 mg (Second Dose)
- Generally Given After Epinephrine if Still in Arrest After Next Rhythm Check
- *See Antiarrhythmic Pharmacology
Adjuncts
- Calcium Chloride
- Dose: 1 g IV
- Vasopressor and Inotropic Effects
- Not Routinely Given but May Be Considered
- Sodium Bicarbonate
- Dose: 50-100 mEq IV (1-2 Amps/Ampules)
- Can Mitigate the Effects of Acidosis and Hyperkalemia
- Not Routinely Given but May Be Considered if Concerned for Significant Acidosis or Hyperkalemia
Cardiac Arrest Management Algorithm:
Immediate CPR and Oxygen
Check Rhythm Every 2 Minutes:
- VF/pVT:
- Defibrillate
- Alternate Epinephrine and Amiodarone After Each Check
- PEA/Asystole:
- Epinephrine After Every Other Check
Adjuncts:
- Calcium Chloride
- Sodium Bicarbonate
Use of Capnography During Cardiac Arrest
- Used to Monitor Adequacy of Compressions:
- Gradual Decline Suggests Decreased Adequacy and Possible Performer Fatigue
- Abrupt Increases Suggest ROSC
- Used After 20 Minutes of CPR to Consider Prognosis:
- ETCO2 > 20 mmHg Has a Higher Chance of ROSC
- ETCO2 < 10 mmHg Has Almost No Chance (0.5%) of ROSC
Post-ROSC (Return of Spontaneous Circulation) Management
- Optimize Oxygenation and Ventilation
- Treat Hypotension (Fluid Bolus, Vasopressors, etc.)
- Obtain a 12-Lead EKG
- STEMI Requires Early Reperfusion Therapy (Percutaneous Coronary Intervention/PCI or Fibrinolysis)
- *See Myocardial Infarction (MI)
- Consider Targeted Temperature Management (TTM) if No Purposeful Neurologic Activity is Seen After ROSC
- *See Therapeutic Hypothermia(TH)/Targeted Temperature Management (TTM)
- Admit to ICU
Special Considerations
Reversible Causes of Sudden Cardiac Arrest: “5 H’s and T’s”
- 5 H’s:
- Hypovolemia
- Hypoxia
- Hydrogen Ions (Acidosis)
- Hypokalemia/Hyperkalemia
- Hypothermia/Hyperthermia
- 5 T’s:
- Tension Pneumothorax
- Trauma and Toxins
- Tamponade (Cardiac)
- Thrombosis (Pulmonary/PE)
- Thrombosis (Coronary/MI)
- “H’s and T’s” are More Often are Associated with PEA Than Asystole
Arrest After Cardiac Surgery
- Assess Rhythm:
- Shockable Rhythms (VF or pVT): Start with Early Defibrillation up to 3x Within 1 Minute Before Starting CPR
- Asystole or Severe Bradycardia: Pace (If Wires Available) and Start CPR
- PEA: Start with CPR and Turn Off Pacer (If Paced) to Exclude Underlying VF
- Additional Considerations:
- Plan Early Emergent Re-Sternotomy with Internal Cardiac Massage
- External CPR Causes More Trauma and Damage to Underlying Bypass Graft
- If IABP in Place, Change to a Pressure Trigger
- CALS Advises Against Full-Dose (1 mg) Epinephrine – Significant HTN Can Harm Fresh Grafts
- Plan Early Emergent Re-Sternotomy with Internal Cardiac Massage
Cardiac Arrest in Trauma
Cardiac Arrest in Pregnancy
