Blunt Thoracic Aortic Injury (BTAI)
Blunt Thoracic Aortic Injury (BTAI)
David Ray Velez, MD
Table of Contents
Background
Significantly High Mortality (80% Pre-Hospital, 20-30% for Those that Survive to the Hospital)
Most Common Mechanism: Motor Vehicle Crash (MVC) (> 70%) – Often Associated with Rapid Deceleration
The Majority (> 60-70%) Occur at the Aortic Isthmus – Just Distal to the Left Subclavian Origin Where the More Mobile Aortic Arch Transitions into the Relatively Fixed Descending Aorta (Additionally the Site of the Ligamentum Arteriosum)
Blunt Mechanisms of Injury
- Crushing Force – Direct Compression Causing Injury
- Shearing Force – Tearing from Acceleration/Deceleration Around Fixed Attachments
- Bursting Force – Force Causing Acutely Increased Intraluminal Pressure with Profound Hypertension Leading to Rupture
Most Have Multiple Associated Injuries (Rib Fracture, Hemothorax, Blunt Cardiac Injury, Blunt Abdominal Trauma, etc.)
Vancouver Classification
- Grade I: Intimal Flap, Thrombus, or Intramural Hematoma < 1 cm
- Grade II: Intimal Flap, Thrombus, or Intramural Hematoma ≥ 1 cm
- Grade III: Pseudoaneurysm
- Grade IV: Free Rupture with Contrast Extravasation
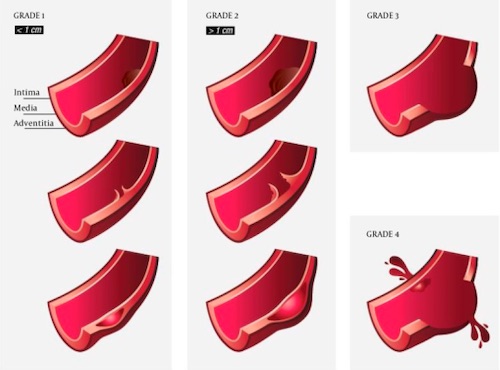
Vancouver Classification of BTAI 1
Diagnosis
Presentation
- Presentation is Generally Nonspecific
- Chest Pain Radiating to the Back
- Shortness of Breath
- Distended Neck Veins
- Absent/Muffled Heart Sounds
- Tracheal Deviation
- Diminished Peripheral Pulses
Diagnosis
- Chest X-Ray (CXR) – Generally the Initial Imaging Modality but Nondiagnostic
- Low Sensitivity (41%)
- Computed Tomographic Angiogram (CTA) – Imaging Modality of Choice for Diagnosis and Classification
- High Sensitivity (95-100%)
- Low Specificity (40%)
- Options if CTA is Equivocal:
- Intravenous Ultrasound (IVUS)
- Catheter Angiography – Historically the Gold Standard in Diagnosis but Now Primarily Used for Therapeutics
CXR Findings Suggestive of Vascular Injury
- Indistinct Aortic Knob
- Wide Mediastinum > 8 cm
- Left Main Bronchus Depression > 140 Degrees
- Deviation of NG/ET Tubes to the Right
- Massive Hemothorax
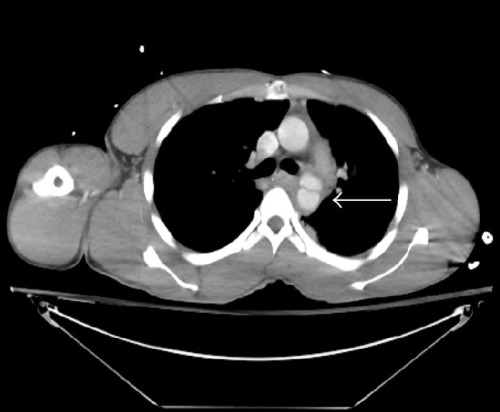
Grade III BTAI – Pseudoaneurysm 2
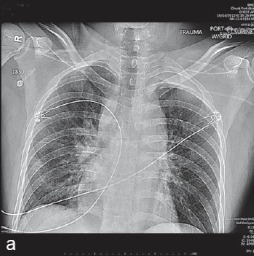
BTAI on CXR (Indistinct Aortic Knob and Widened Mediastinum 3
Management
If History and Physical Exam is Suggestive of Blunt Thoracic Aortic Injury Start Anti-Impulse Therapy if Otherwise Stable, Even Before Definitive Diagnosis
Anti-Impulse Control
- The Primary Goal is to Reduce Aortic Wall Stress and Prevent Lesion Progression
- Goals Parameters:
- Systolic Blood Pressure (SBP) ≤ 100 mmHg
- Mean Arterial Pressure (MAP) ≤ 80 mmHg
- Heart Rate (HR) ≤ 100 bpm
- Most Often Achieved with a Rapid-Acting Beta-Blocker (Esmolol or Labetalol)
- Decreases Risk of Rupture from 12% to 1.5%
Grade I: Anti-Impulse Control Alone
- Some Also Recommend Medical Management Alone for Grade II Injuries (Controversial)
- Progression of Minor Injuries (Grade I-II) are Rare (5-7%) and Often Completely Resolve with Time
Grade II-IV: Anti-Impulse Control and Repair
- Ascending Aorta/Aortic Arch: Open Surgical Repair
- Descending Aorta: Thoracic Endovascular Aortic Repair (TEVAR)
- Lower Mortality, Blood Loss, and Paraplegia Risk Than Open Repair
- Shorter Graft Length May Help to Decrease Risk of Spinal Cord Ischemia and Paraplegia
- May Require Coverage of the Left Subclavian Artery for an Adequate Proximal Landing Zone (Covered in Up to 40% of Repairs) – Appears to Be Safe and Does Not Compromise Functional Outcomes
References
- Forcillo J, Philie M, Ojanguren A, Le Guillan S, Verdant A, Demers P, Lamarche Y. Outcomes of Traumatic Aortic Injury in a Primary Open Surgical Approach Paradigm. Trauma Mon. 2015 May;20(2):e18198. (License: CC BY-NC-4.0)
- Chen C, Schuster K, Bhattacharya B. Motor vehicle collision patient with simultaneous duodenal transection and thoracic aorta injury: a case report and review of the literature. Case Rep Surg. 2015;2015:519836. (License: CC BY-3.0)
- Alameddine AK, Alimov VK, Alvarez C, Rousou JA. Unexpected traumatic rupture of left atrium mimicking aortic rupture. J Emerg Trauma Shock. 2014 Oct;7(4):310-2. (License: CC BY-NC-SA-3.0)
