Arterial Line (A-Line)
Arterial Line (A-Line)
David Ray Velez, MD
Table of Contents
Indications and Site Selection
Indications
- Continuous Blood Pressure Monitoring – The Primary Indication and Use
- Hemodynamic Instability
- Titration of Vasoactive Agents
- Morbid Obesity and Unable to Use a Non-Invasive Blood Pressure (NIBP) Cuff
- Frequent Blood Sampling
- Arterial Drug Administration
- Use of an Intra-Aortic Balloon Pump (IABP)
Site Selection
- Radial Artery – Generally the Preferred Site if Able
- Femoral Artery
- Axillary Artery
- Brachial Artery – Worst Choice (Highest Risk for Distal Ischemia)
- Dorsalis Pedis – Generally Only Used in Children
Allen Test
- A Procedure to Evaluate the Adequacy of Collateral Blood Flow to the Hand Before Arterial Line Placement to Prevent Hand Ischemia
- Technique:
- Manually Occlude Radial and Ulnar Arteries
- Clench Hand 10-Times
- Release Ulnar Artery While Still Occluding the Radial Artery
- Monitor Capillary Refill
- Interpretation:
- Negative: Capillary Refill > 6 Seconds
- Indicates Inadequate Contralateral Flow
- Positive: Capillary Refill < 6 Seconds
- Indicates Adequate Contralateral Flow
- Negative: Capillary Refill > 6 Seconds
- Use in Practice is Debated Due to Poor Accuracy and Interobserver Agreement
Technique
Techniques
- Blind Placement: Based Solely on Anatomy and Palpation without US Guidance
- Ultrasound Guidance: Placed Using an Ultrasound in Real-Time
- Benefits to Ultrasound Use:
- Increased First-Pass Success
- Decreased Complication Rate
- Decreased Failure Rate
- Should Always be Utilized if Available
- Benefits to Ultrasound Use:
- *Either Method Utilizes a Seldinger Technique
Position/Prep – Radial Artery
- Use a Flexible Board or Rolled Towel to Stabilize the Wrist in Dorsiflexion
- Extension of the Wrist to 45-Degrees Increases Anterior-Posterior Arterial Diameter and Success Rate
- Procedure Should be Performed in a Sterile Manner Unless Absolutely Unable (“Dirty Lines” Used in Trauma for a Crashing Patient in Hemorrhagic Shock)
- Consider Performing an Allen Test Prior to Placement – Debated
- Inject Local Anesthetic as Appropriate
Position/Prep – Axillary Artery
- Anterior Chest Approach:
- Supine with Arms Tucked (Similar to a Subclavian Approach)
- Vessels Located Between the Crease of the Arm and Clavicle in the Deltopectoral Groove
- Axillary Approach:
- Open the Axilla by Abduction and External Rotation of the Arm 90-135 Degrees
- May Need to Shave Axilla
- Take Caution to Approach Medially Enough to Avoid the Brachial Artery
- Procedure Should be Performed in a Sterile Manner Unless Absolutely Unable (“Dirty Lines” Used in Trauma for a Crashing Patient in Hemorrhagic Shock)
- Inject Local Anesthetic as Appropriate
Seldinger Technique
- Needle
- Puncture the Artery with a Hollow Introducer Needle
- Needle is Generally Not Attached to a Syringe and Rather Left Open to Monitor Pulsation
- Bright Red Pulsatile Blood Indicates Arterial Puncture
- Guidewire
- Pass a Guidewire Through the Needle
- Withdraw the Needle Over the Guidewire, Leaving the Guidewire in Place
- Always Maintain Control of the Guidewire During Placement – Should Never Completely Enter the Artery
- Place the Catheter
- Make a Small Skin Incision at the Entry Site
- Do Not Need to Dilate the Tract
- Pass Catheter Over the Guidewire
- Withdraw Guidewire
- Attach the Catheter to the Monitor and Confirm Waveform
- Suture Catheter to the Skin and Place a Sterile Dressing
Seldinger Technique – Dart/Arrow Kit
- *A Vascular Access Device Kit with a 20 Gauge Angiocatheter and a Preloaded Wire within a Plastic Tube
- *Only Used in the Radial Artery
- Needle
- Puncture the Radial Artery with the Dart Needle
- Bright Red Pulsatile Blood into the Tubing Indicates Arterial Puncture
- Guidewire/Catheter
- Pass the Guidewire Through the Needle
- Advance the Catheter Over the Guidewire
- Withdraw the Guidewire/Needle, Leaving the Catheter
- Attach the Catheter to the Monitor and Confirm Waveform
- Suture Catheter to the Skin and Place a Sterile Dressing
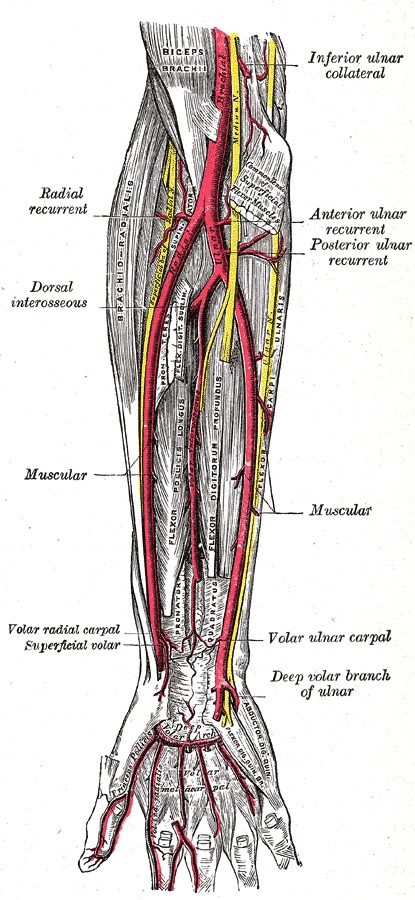
Radial Artery
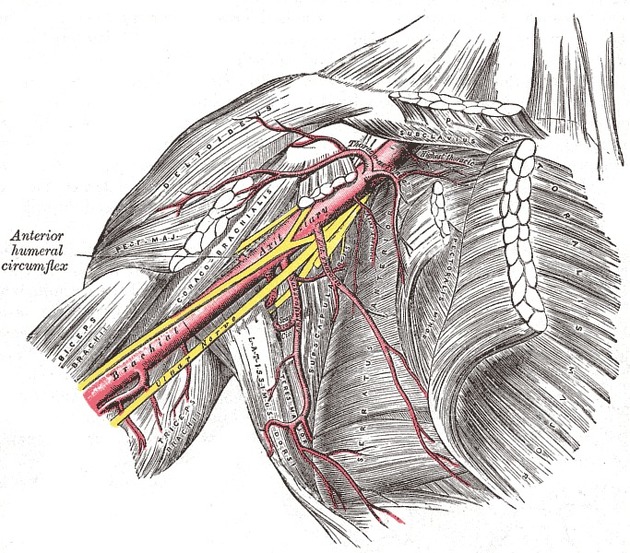
Axillary Artery: Outer Border of the First Rib to the Lateral Border of the Teres Major
Arterial Waveform Analysis
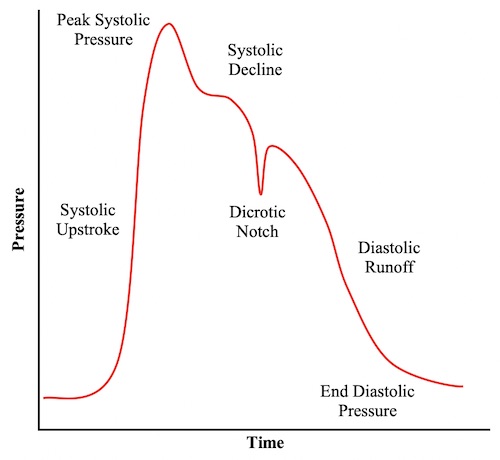
Arterial Waveform
- Systolic Upstroke: Systolic Ventricular Ejection
- Systolic Decline: Beginning of Decline Before Diastole
- Dicrotic Notch: Closure of Aortic Valve (Start of Diastole)
- Diastolic Runoff: Decline During Diastole
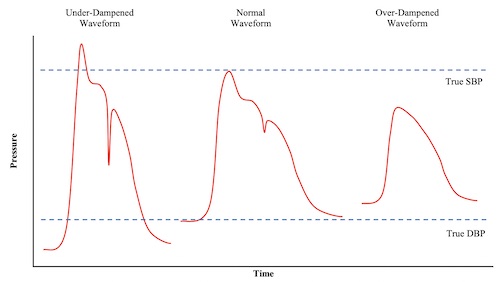
Under-Dampened System
- Definition: Waveform Appears Saltatory and Abrupt with an Exaggerated Dicrotic Notch
- Pressure Changes:
- Increased Systolic Blood Pressure (SBP)
- Decreased Diastolic Blood Pressure (DBP)
- Increased Pulse Pressure
- Causes:
- Excessively Long Tubing Length
- Multiple Stopcocks
Over-Dampened System
- Definition: Waveform Appears Flattened with a Small Amplitude and Loss of the Dicrotic Notch
- Pressure Changes:
- Decreased Systolic Blood Pressure (SBP)
- Increased Diastolic Blood Pressure (DBP)
- Decreased Pulse Pressure
- Causes:
- Air Bubbles in the Tubing
- Arterial Thrombus
- Tube Kinging
Arterial Waveform
System Dampening
Complications
Bloodstream Infection (BSI)
- Incidence: 1.6 Infections/1,000Catheter Days
- Similar Risk as Short-Term Central Venous Catheters (CVC) Despite Dogma that States Arterial Lines Rarely Get Infected
- Most Common Source: Skin Colonization
- Most Common Organism: Staphylococcus epidermidis
- Highest Risk Site: Femoral Artery
- Chlorhexidine Impregnated Dressings (BioPatch) Decrease the Risk
- Full Barrier Precautions May Not Decrease the Risk Compared to Sterile Gloves Alone for Radial Lines – Minimal Data to Support/Reject
Hand Ischemia After Radial Artery Catheterization
- Thrombosis/Temporary Arterial Occlusion is the Most Common Complication of Radial Artery Catheterization (20-33%)
- Clinically Significant Ischemia is Rare (< 0.1%)
- Brachial Artery is the Highest Risk Site
- Risk Factors:
- Low BMI
- Female Gender
- Advanced Age
- Vascular Disease
- Vasopressor Use
- Prolonged Hypotension
- Larger Catheter Size
- Prolonged Catheter Placement (> 48-72 hr)
- Trauma from Multiple Attempts at Placement
- General Management: Remove Catheter and Anticoagulation
- May Require Surgical Intervention (Embolectomy, Bypass, or Amputation)
Other Complications
- Bleeding/Hematoma
- Pseudoaneurysm
- Vasospasm
