Air Embolism
Air Embolism
Brenna C Chen, MD
Table of Contents
Definition
Definition: Abnormal Collection of Gas that Forms a Bubble in the Bloodstream and Circulatory System
Venous Air Embolism (VAE): Abnormal Collection of Gas that Forms a Bubble within the Venous System
Arterial Air Embolism (AAE): Abnormal Collection of Gas that Forms a Bubble within the Arterial System
- Less Common than Venous Air Embolism
- Generally a More Critical and Damaging Condition than Venous Air Embolism
Pathophysiology
Venous Air Embolism (VAE)
- Venous Air Follows One of Three Pathways
- Passes Through the Right Heart and into the Pulmonary Circulation
- Passes Through the Inferior Vena Cava (IVC)/Hepatic Veins into the Liver
- Ascends Superiorly Through the Superior Vena Cava (SVC)/Jugular Veins Causing a Cerebral Air Embolism – More Common with Larger Emboli
- Air May Collect in the Main Pulmonary Artery or Right Ventricle Leading to Obstruction of the Pulmonary Outflow Tract (Referred to as “Air Lock”)
- Occurs with Larger Emboli, Usually Greater Than 50 cc
- Causes Increased Central Venous Pressure and Decreased Pulmonary and Systemic Arterial Pressure
- Air Emboli Small Enough to Enter the Pulmonary Arterioles Can Cause Pulmonary Edema Leading to Histamine and Serotonin Release, Pulmonary Vasoconstriction, and Increased Capillary Permeability
- Emboli that Enter the Arterial Circulation Can Cause Ischemia
Arterial Air Embolism (AAE)
- Sources:
- Air Directly Introduced into the Arterial System
- Venous Air Embolism that Enters Arterial Circulation by Either Overwhelming Pulmonary Circulation or Via Right-to-Left Shunt (Referred to as “Paradoxical Embolism”)
- Lethal Volume: 3-5 mL/kg or 300-500 mL at a Rate of 100 mL/s
- Can Cause Ischemia in Any Organ with Insufficient Collateral Circulation
- Cerebrovascular Accident (CVA)
- Mesenteric Ischemia
- Acute Limb Ischemia
- Myocardial Infarction (MI)
- Air in the Pulmonary Artery:
- Causes Increases Pulmonary Artery/Right Ventricular Pressure Which Can Cause Right Heart Strain, Reduced Cardiac Output, and Arrhythmia
- Causes a Ventilation Perfusion (V:Q) Mismatch
- Air in the Left Ventricle Causes Reduced Diastolic Filling and Cardiovascular Compromise
Causes
The Majority of Cases are Due to Iatrogenic Causes
Venous – Iatrogenic Causes
- Central Venous Catheterization – The Most Common Cause
- Can Occur During Placement, Usage, or Removal
- Pressurized Intravenous Infusions
- Hemodialysis
- High Pressure Mechanical Ventilation (Barotrauma)
- Surgical Procedures:
- Head And Neck Surgery
- Neurosurgical Procedures
- Cardiovascular Surgery
- Resuscitative Thoracotomy
- Thoracentesis
- Transplant Surgery
- Laparoscopic Procedures
- Arthroscopy
- Obstetric and Gynecologic (OBGYN) Procedures
Venous – Non-Iatrogenic Causes
- Blunt or Penetrating Chest Trauma
- Diving – Rapid Ascent Can Cause Dissolved Gas to Expand and Form Bubbles
Arterial – Iatrogenic Causes
- Paradoxical Air Embolism (Venous Air Emboli that Enter the Arterial System)
- Arterial Catheterization
- Cardiopulmonary Bypass
- Percutaneous Lung Biopsy
Arterial – Non-Iatrogenic Causes
- Paradoxical Air Embolism (Venous Air Emboli that Enter the Arterial System)
- Diving – Rapid Ascent Can Cause Dissolved Gas to Expand and Form Bubbles
Presentation and Complications
Most Commonly Presents with Hypoxemia and Respiratory Distress
Cardiac
- “Mill-Wheel” Murmur (Loud Churning) – A Late Finding
- Arrhythmia
- Elevated Jugular Venous Pressure (JVP)
- Hypotension
- Myocardial Infarction (MI) – Rare and Usually Due to Air Entrance into the Arterial System Through a Congenital Heart Defect
- Cardiac Arrest
Pulmonary
- Chest Pain
- Shortness of Breath
- Tachypnea
- Respiratory Distress/Failure
- Hemoptysis
Neurologic
- Neurologic Deficits – Primarily if Embolized to the Arterial System
- Altered Mental Status (AMS)
- Transient Ischemic Attack (TIA)
- Cerebrovascular Accident (CVA)
- Seizures
Other Complications
- Acute Kidney Injury (AKI)
- Death – Overall Mortality Rate Around 21%

Mill Wheel 1

CT Showing Air Embolism in the Left Middle Cerebral Artery Distribution (Arrow) Causing Stroke 2
Diagnosis
Diagnosis is Confirmed by the Demonstration of Intravascular Air with a Known Risk Factor
- Air is Often Rapidly Absorbed Before Imaging Can Be Performed
Labs
- Labs are Generally Non-Specific
- Arterial Blood Gas (ABG) May Show Hypercapnia, Hypoxemia, and Metabolic Acidosis (If Venous) or Respiratory Alkalosis (If Arterial)
Imaging
- Transesophageal Echocardiography (TEE) – May Visualize Air Within the Heart
- The Most Sensitive Test Overall
- CT Scan – May Visualize Air Within Blood Vessels
- Precordial Doppler Monitoring – A Doppler US Probe Placed Over the Chest to Monitor for Changes in Signal Blood Flow Indicating Venous Air Embolism During Surgery (Particularly Used During Neurosurgery)
- The Most Sensitive Non-Invasive Test for Venous Embolism
End Tidal Nitrogen (If Available and Rarely Performed) Rises Before End Tidal CO2 Decreases
EKG and Troponins are Not Specific for Air Embolism but Can Evaluate for Coronary Ischemia or Arrhythmia
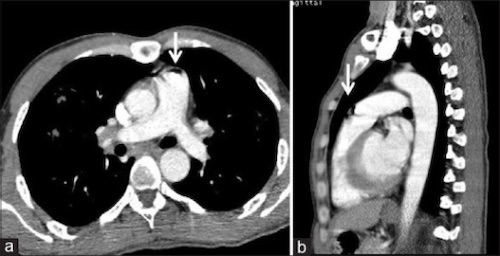
Air Embolism (Arrow) in the Pulmonary Artery 3
Treatment
Management is Mostly Supportive
Venous Air Embolism (VAE)
- The First Step if Concerned Should Be Repositioning Even Before the Diagnosis is Made
- Management is Mostly Supportive with Supplemental Oxygen (100% FiO2) and Positioning
- Repositioning: Left Lateral Decubitus (Durant’s Maneuver) AND Trendelenburg Position
- Goal: Positioning to Trap Air in the Right Ventricle and Prevent Spread
- The Term “Durant’s Maneuver” Specifically Refers to Left Lateral Decubitus (Left-Side Down) Although it is Often Mistakenly Described as Both Left Lateral Decubitus AND Trendelenburg Positioning
- Secondary Options if Hemodynamically Unstable:
- Aspiration Through a Central Venous Catheter if Already in Place
- Hyperbaric Oxygen
- Cardiac Massage (Chest Compressions) to Force Air into Smaller Vessels
Arterial Air Embolism (AAE)
- Maintain Supine Positioning (Do NOT Place in Left Lateral Decubitus or Trendelenburg – Can Exacerbate Symptoms)
- Management is Mostly Supportive with Supplemental Oxygen (100% FiO2)
- IV Fluids or Vasopressors if Hypotensive
- Hyperbaric Oxygen if Has Hemodynamically Instability, Neurologic Deficits, or Signs of End Organ Damage
- Goal: Reduces Size of Air Emboli to Promote Reabsorption
- Can Attempt Aspiration Through the Catcher if it Occurs During Angiography
- Consider Nitroglycerin if Involving the Coronary Arteries
References
- Dace A. Wikimedia Commons. (License: CC BY-SA-2.0)
- Delaney MC, Bowe CT, Higgins GL. Acute stroke from air embolism after leg sclerotherapy. West J Emerg Med. 2010 Sep;11(4):397. (License: CC BY-NC-4.0)
- Sodhi KS, Saxena AK, Chandrashekhar G, Bhatia A, Singhi S, Agarwal R, Khandelwal N. Vascular air embolism after contrast administration on 64 row multiple detector computed tomography: A prospective analysis. Lung India. 2015 May-Jun;32(3):216-9. (License: CC BY-NC-SA-3.0)
