Pleural Effusion
Pleural Effusion
David Ray Velez, MD
Table of Contents
Definition
Pleural Effusion Definition: Fluid within the Pleural Space
Types
- Transudative Pleural Effusion: From Unbalanced Hydrostatic and Osmotic Pressures
- Results in Smaller Proteins
- Exudative Pleural Effusion: From Inflammation Increasing Capillary Permeability
- Results in Larger Proteins
Causes
Transudative Pleural Effusion
- Congestive Heart Failure (CHF) – The Most Common Transudative Cause
- Atelectasis
- Hepatic Hydrothorax
- Hypoalbuminemia
- Nephrotic Syndrome
Exudative Pleural Effusion
- Malignancy – The Most Common Exudative Cause
- Hemothorax (HTX)
- Parapneumonic Effusion or Empyema
- Chylothorax
- Amyloidosis
- Sarcoidosis
- Pulmonary Embolism
Pleural Fluid Physiology
Function
- Serous Fluid
- Acts as a Lubricant for the Parietal and Visceral Pleura
- Prevents Adhesion During Respiration
Flow
- Production: Parietal Circulation (Intercostal Arteries) from Bulk Flow
- Reabsorption: Lymphatic System
- Mostly (75%) from Lymphatics of the Parietal Pleura
- Visceral Pleural Plays No Significant Role in Drainage
The Parietal Pleura is the Primary Determinant of Fluid Turnover
Volume
- Normal Volume: 10-20 cc
- Fluid Turnover Ability: 1-2 L/Day
- Can Increase Up to 40x Normal Rates
- Requires a Profound Increase in Production or Blockage of Lymphatics to Initiate Fluid Accumulation
Diagnosis
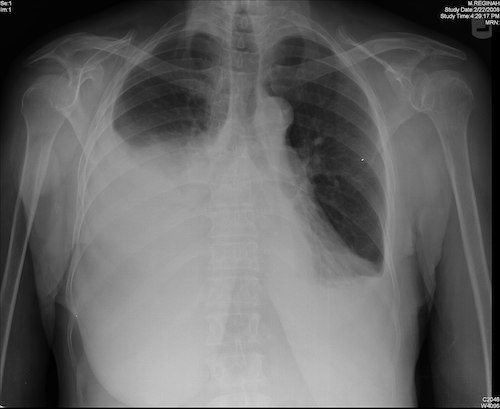
Generally a Radiographic Diagnosis (CXR, CT, or POCUS)
- Minimum Volume Required to Be Seen on a Standard Upright PA CXR: 300 cc
Differential Evaluation
- Thoracentesis and Pleural Fluid Evaluation
- Routine Orders:
- Cell Count/Differential
- pH
- Protein (Pleural and Serum)
- LDH (Pleural and Serum)
- Also Consider:
- Glucose
- Amylase
- Cholesterol
- Triglycerides
- Bacterial Culture
Light’s Criteria
- Indicates that the Effusion is Exudative
- Criteria (Requires ≥ One):
- Pleural:Serum Protein Ratio > 0.5
- Pleural:Serum LDH > 0.6
- Pleural LDH > 2/3 the Upper Limit of Normal
Three-Test Rule
- Indicates that the Effusion is Exudative
- Criteria (Requires ≥ One):
- Pleural Protein > 2.9 g/dL
- Pleural Cholesterol > 45 mg/dL
- Pleural LDH > 0.45x the Upper Limit of Normal
| Transudate | Exudate | |
| WBC | < 1,000 | > 1,000 |
| pH | 7.40-7.55 | 7.30-7.45 |
| Pleural:Serum Protein Ratio | < 0.5 | > 0.5 |
| Pleural:Serum LDH Ratio | < 0.6 | > 0.6 |
| Cholesterol | < 45 mg/dL | > 45 mg/dL |
Specific Measures
- Complicated Parapneumonic Effusion/Empyema: WBC > 50,000 and pH < 7.30
- Chylothorax: Triglycerides > 110 mg/dL
Pleural Effusion 1
Treatment
Treat Any Underlying Disorder
Fluid Drainage
- Asymptomatic: Generally No Drainage Required
- Symptomatic: Thoracentesis vs. Thoracostomy Tube (Chest Tube)
- *See Thoracostomy Tube (Chest Tube)
- Thoracentesis Improves Oxygenation but No Significant Effect on A-a Gradient, LOS, or Mortality
- Stop Immediate Drainage if Having Pain or Total Fluid > 1.0-1.5 L
- At Risk for Re-Expansion Pulmonary Edema When Larger Volumes are Drained
- If Fails: Thoracoscopic Talc Pleurodesis vs Long-Term Drainage
Malignant Pleural Effusion (MPE): Indications for a Tunneled Pleural Catheter
- Recurrent Symptomatic Fluid Build-Up
- Short Life-Expectancy (< 3 Months)
- Poor Functional Status
- Trapped Lung
- Bulky Pleural Metastases
- Failed Pleurodesis
- Patient Preference Over Repeated Thoracentesis or Surgical Intervention
References
- Rosen Y. Wikimedia Commons. (License: CC BY-SA-2.0)
